An analysis of the effects of neurodiversity on health, and vice versa.
Grade 10
Presentation
Problem
The area of the health effects of neurodivergence has not been studied enough, and could help medical professionals with diagnoses of conditions in neurodivergent individuals because the data could show that neurodivergence makes some conditions more likely. This could also pave the way for further research into why this happens, granting us further knowledge of neurodivergence and conditions that may prove to be associated with it. But this is not it, maybe findings will support that other health areas, physical and mental, could even drive neurodivergence.
Method
Participants were recruited through a poster I made in canva, with a QR code linking to a Microsoft Form, the exact questions in that form are in the "Attachments" section. Data collection was between November 19th, 2024, and March 1st, 2025, and thus lasted 102 days, I shared the poster with my psychologist, who in turn shared it with her colleagues, my Mom also distributed the poster. The data was analyzed manually by me, using a spreadsheet made by my Mom and Dad (I don't know how to use excel), with graphs made when appropriate.
Research
Abstract
This study had 29 participants with 26 usable responses, each are neurodivergent in different ways and submitted an online form about their health in specific areas (neurological and psychiatric; genetic and mitochondrial conditions, and conditions of the digestive system) with a section for other conditions not in said areas. Findings showed various neurological and psychiatric disorders had higher prevalence in the sample group, as did digestive conditions, particularly variations of irritable bowel syndrome (IBS). The intent of the study is to determine the effects of neurodivergence on health, but it may have found an effect of health on neurodiversity, as IBS was unusually common in the sample.
Introduction
Not much is known about the cause of disorders that result in neurodivergence, or what those disorders can mean for the rest of the body. It is with this in mind that this study hopes to shed some light on such things. An initial hypothesis is that psychiatric, neurological, mitochondrial, genetic, and digestive system conditions might be more prevalent in neurodivergent individuals. The reasons for these specific areas of focus are that psychiatric and neurological conditions also arise from the brain, and may be corellated as such, genetics have shown to play a role in the prevalence of conditions like autism spectrum disorder (ASD)[1]. Mitochondria have shown to be related as well[2], and due to the gut-brain axis, I have decided to investigate the digestive system as well.
Methods
See methods.
Raw Data
See data.
Analysis
See data.
Conclusion
See conclusion.
Data
Raw Data
All data can be found is this Excel spreadsheet: https://1drv.ms/x/c/28e3247ab89cac1b/Eesa13_LwupCvNj46rz8zwUBNEfut-My72XKa3mJNMhsvg
Graphs:
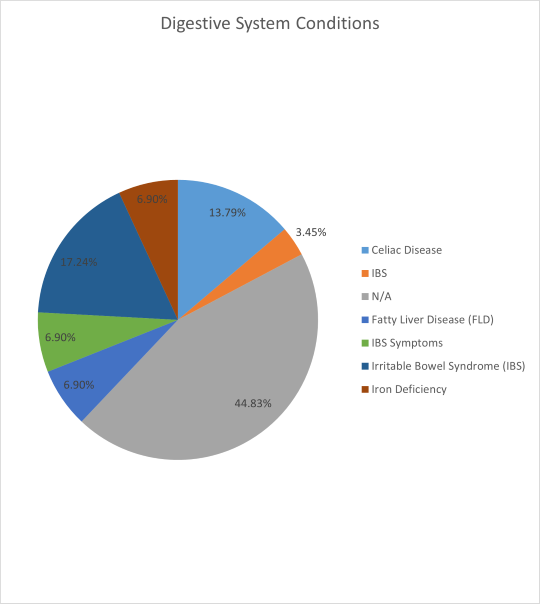
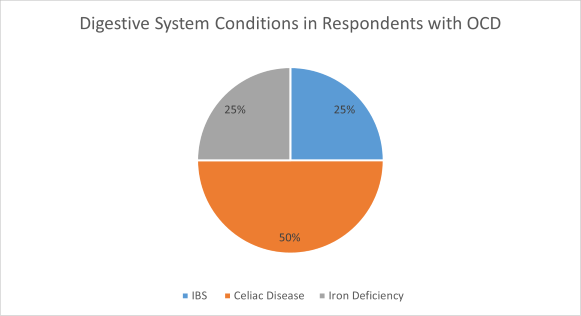
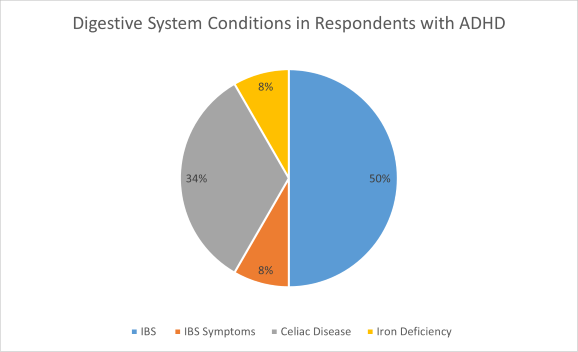
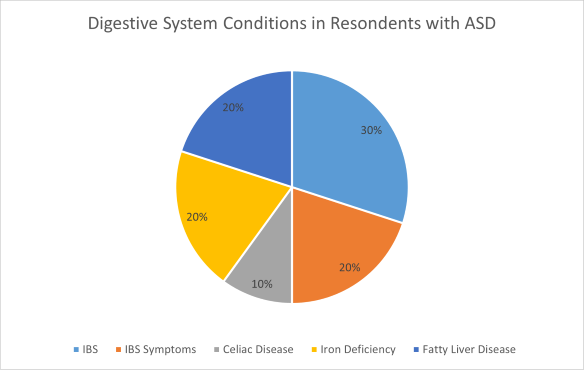
If segment is unlabeled, it is N/A.
Analysis
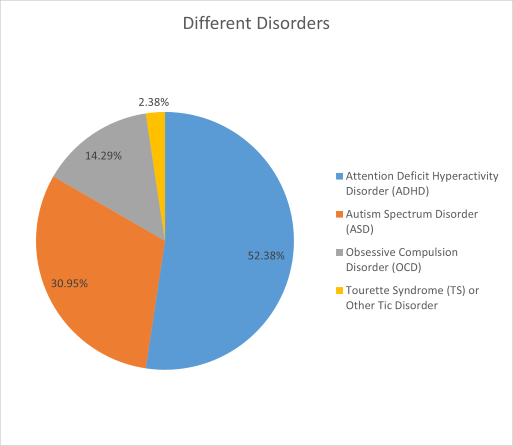
The sample was made of 26 individuals with usable responses, of them, 52.38% (21 respondents) of reported disorders were ADHD, 30.95% (13 respondents) of reported disorders were ASD, 14.29% (6 respondents), of reported disorders were OCD, and 2.38% (1 respondent) of reported disorders were TS or another tic disorder. The TS or other tic disorder datapoint will not be considered in its own category, due to the small sample size.
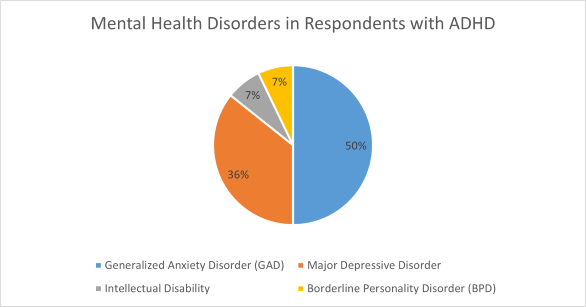
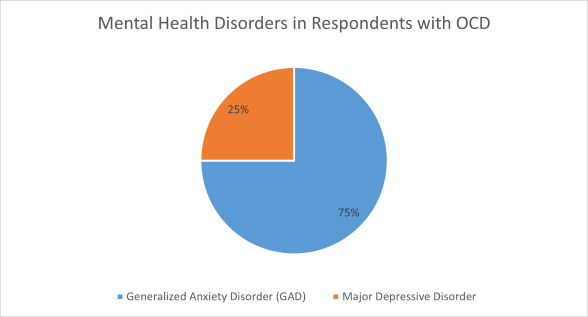
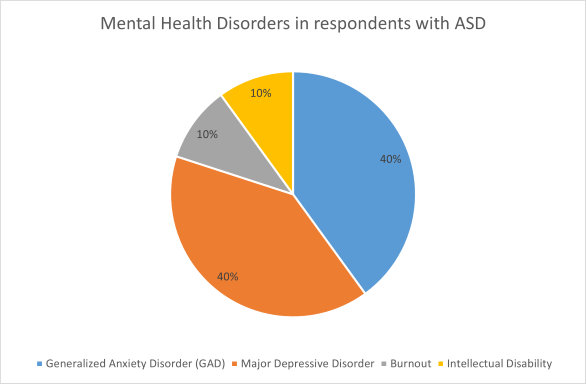
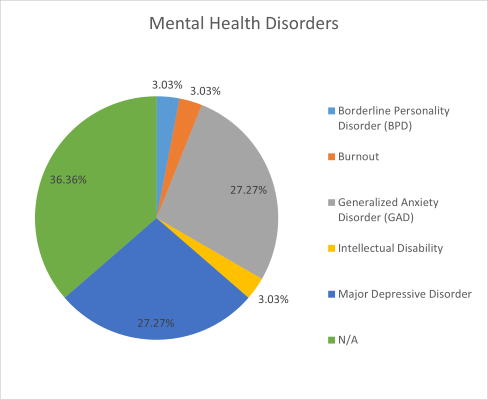
Mental health disorders other than those that are the cause of neurodivergence were quite common across the sample as a whole, as well as the groups divided by initial condition, which makes sense given that these disorders appear often in the general population[3][4], but these rates are higher suggesting a correlation. Due to the way these disorders causing neurodivergence affect the mind, it is my hypothesis that such disorders as ADHD, ASD, and OCD predispose an individual to these pathologies. Major depressive disorder and GAD were the most common across the whole sample, GAD was more common in the OCD and ADHD groups than depression, and GAD and depression were equal in occurrence in the ASD group. This suggests that GAD and major depressive disorder are those with the highest correlation, with individuals who have OCD or ADHD being more vulnerable to GAD than depression, with depression still at concerning levels, while the ASD group is probably equally predisposed to them both. The ramifications here could be that a physician may consider these diagnoses more in depth or often, due to the possible predisposition. This also leads me to ask the question of whether these 2 disorders are more severe in neurodivergent individuals, to answer this question, more research is required.
Digestive system conditions were included not due to the affects of neurodiversity on them, but because they may contribute to neurodiversity. A concept gaining traction currently is the gut-brain axis (GBA), which as the name suggests, is a way in which the gastrointestinal tract influences the brain, and vice versa. The neural connections between the central and enteric nervous systems allow each end to affect the other, but the gut is also influenced by its microbiome, allowing the brain and gut microbiota to indirectly interact (further reading on the GBA in citation[5]). In the sample, IBS rates including IBS symptoms without a diagnosis, were on par with the global average[6], but the ASD and ADHD groups had rates much higher (also counting just symptoms). The cause of IBS is not known, but is has been linked to the GBA[7]. This may even signal a causal relationship where IBS is directly linked to neurodivergence. More research is needed to confirm such a hypothesis, but this data could help to influence the differential diagnosis of the physician caring for a neurodivergent patient.
Conclusion
In conclusion, this study has investigated the effects of neurodiversity on health, and vice versa, on a sample of 26 individuals, with 3 being removed to get to that number. Generalized anxiety disorder, major depressive disorder, and irritable bowel syndrome and its symptoms, have shown to be common in the sample, with different amounts in different subgroups. From my analysis of the data, conclusions can be drawn that neurodivergence predisposes an individual to GAD and depression, and that IBS may be linked to neurodiversity in a way such that IBS may influence neurodivergence. The ramifications of this study could have profound implications, it could direct future research towards understanding what drives neurodiversity, and it can improve the healthcare of neurodiverse individuals by assisting the physician in diagnosing their patients problems. Ultimately, more research is required, but I believe this is a great start towards the original problem.
Citations
Thiese MS. Observational and interventional study design types; an overview. Biochem Med (Zagreb). 2014;24(2):199-210. doi: 10.11613/BM.2014.022. Epub 2014 Jun 15. PMID: 24969913; PMCID: PMC4083571.
STROBE study checklist V4 Combined, could not properly link, STROBE's website is here: https://www.strobe-statement.org. This was used to loosely guide the writing of the article.
[1] de la Torre-Ubieta L, Won H, Stein JL, Geschwind DH. Advancing the understanding of autism disease mechanisms through genetics. Nat Med. 2016 Apr;22(4):345-61. doi: 10.1038/nm.4071. PMID: 27050589; PMCID: PMC5072455.
[2] Rojas-Charry L, Nardi L, Methner A, Schmeisser MJ. Abnormalities of synaptic mitochondria in autism spectrum disorder and related neurodevelopmental disorders. J Mol Med (Berl). 2021 Feb;99(2):161-178. doi: 10.1007/s00109-020-02018-2. Epub 2020 Dec 18. PMID: 33340060; PMCID: PMC7819932.
[3]Ruscio AM, Hallion LS, Lim CCW, et al. Cross-sectional Comparison of the Epidemiology of DSM-5 Generalized Anxiety Disorder Across the Globe. JAMA Psychiatry. 2017;74(5):465–475. doi:10.1001/jamapsychiatry.2017.0056
[4]Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AT. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122:184-191.
Cover Image:
OpenAI. “Digital Cover Image Illustrating the Relationship Between Neurodiversity and Health.” DALL·E via ChatGPT, 18 Mar. 2025.
Header image:
https://commons.wikimedia.org/wiki/File:Neurodiversity_Crowd_2.png
[5]Mayer EA, Nance K, Chen S. The Gut-Brain Axis. Annu Rev Med. 2022 Jan 27;73:439-453. doi: 10.1146/annurev-med-042320-014032. Epub 2021 Oct 20. PMID: 34669431.
[6]Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014 Feb 4;6:71-80. doi: 10.2147/CLEP.S40245. PMID: 24523597; PMCID: PMC3921083.
[7]Hillestad EMR, van der Meeren A, Nagaraja BH, Bjørsvik BR, Haleem N, Benitez-Paez A, Sanz Y, Hausken T, Lied GA, Lundervold A, Berentsen B. Gut bless you: The microbiota-gut-brain axis in irritable bowel syndrome. World J Gastroenterol. 2022 Jan 28;28(4):412-431. doi: 10.3748/wjg.v28.i4.412. PMID: 35125827; PMCID: PMC8790555.
Acknowledgement
I was far from the only one involved in this project. I would like to thank my Dad, Greg Babuk, for his tech support relating to anything I couldn't figure out, my Mom, Stephanie Babuk, for helping spread the poster and with using Excel, my psychologist, Laurel York, for sharing the poster and advising me, my tutor, Jenna Lehocky, for help proofreading, my grandfather, Tom Babuk, for proofreading (he spotted a rounding error in one of my graphs, it's still there, by the way), Jessica Sung, the teacher in charge of the science fair club, for her help brainstorming, coordinating, and getting me into this all, and finally, the anonymous respondents to the survey (and Caleb, because I know he did it), for giving me the data I needed to bring this to life. This would not have happened without you all, thank you for your help.

