Endometriosis Treatment: Robotized?
Grade 8
Presentation
Problem
What are the comparative outcomes and advantages of robotic surgery versus conventional laparoscopic surgery for the treatment of endometriosis in terms of operating time, blood loss, length of hospital stay, and complication rate?
Method
Search Strategy
A search of 4 electronic databases was conducted (PubMed, Embase, Scopus, CINAHL). All English publications comparing RAS and LPS for the treatment of endometriosis from January 2001 to September 2023 were identified. The following keywords were used in the search: “endometriosis” AND “laparoscopic surgery” AND “robotic”. This search was modified, and other search terms were used, such as “laparoscopy”, and “robotic surgery” in the place of “laparoscopic surgery” and “robotic”, respectively. However, the first search query was most commonly used. Related articles provided by the databases were also searched.
Data was extracted by one independent researcher. PRISMA guidelines were used.
Inclusion Criteria
All of the studies that were included in the review met the following criteria: directly compared LPS and RAS in patients with endometriosis, addressed one or more of the outcome measures of operating time, blood loss, complication rate, or length of hospital stay, had a sample size of more than 25, English-language sources, and had easily accessible full-text versions.
Exclusion Criteria
Sources that only reported LPS or RAS were excluded. Studies that did not focus on endometriosis were excluded. Sources in languages other than English or those without full-text versions were also excluded. Publications that didn’t provide clear information about patients or results were excluded.
Research
Background Research
What is Endometriosis?
Endometriosis is a chronic disease that occurs when endometrial-type tissue grows outside of the uterus and on other areas of the body. The new endometrium is grown with the menstrual cycle; however, in individuals with endometriosis, the body cannot shed the endometrium that is outside the uterus. This inability causes a buildup of abnormal tissue, leading to inflammation, scarring, and cysts. Additionally, endometriosis can make the reproductive tissue “stick” together due to a buildup of fibrous tissues. This condition affects approximately 10% of reproductive-aged women, and there is currently no known cure. Treatments are usually focused on symptom control.
Stages of endometriosis:
|
Stage |
Description |
Characteristics |
Point Score Range |
|
I |
Minimal endometriosis |
- Superficial implants and mild adhesions |
1 to 5 |
|
II |
Mild endometriosis |
- Superficial or deep implants with mild adhesions - Widespread endometriosis with deep implants |
6 to 15 |
|
III |
Moderate endometriosis |
- Deep implants present - Dense adhesions - Widespread endometriosis |
16 to 40 |
|
IV |
Severe endometriosis |
- Deep implants and dense adhesions present - More widespread disease than in Stage III - Indicates severe endometriosis |
Greater than 40 |
Four types:
Superficial endometriosis is predominantly found in the pelvic peritoneum. The pelvic peritoneum is a crucial membrane lining the abdominal pelvic cavity, and plays a multifaceted role in surrounding and safeguarding abdominal organs. Its functions extend to holding these organs in place and secreting lubricating fluid to mitigate friction during their interactions.
Cystic ovarian endometriosis, also known as endometriomas, manifests within the ovaries. These structures, vital for reproductive health, become affected by the abnormal growth of endometrial tissue. Can occur with other forms of endometriosis.
Deep infiltrating endometriosis (DIE) infiltrates other organs such as the bladder, bowel, and recto-vaginal septum. This deeper involvement introduces complexities and potential complications, impacting various bodily functions.
Beyond the pelvis, instances of endometriosis are exceptionally rare.
Some Key Terms:
|
Term |
Description |
Characteristics |
|
Endometriosis Implants |
Endometrial cells growing outside the uterus |
- Typically grow outside the uterus - Spread and grow outside the uterus - Small and flat lesions |
|
Endometrial Adhesions |
Clusters of fibrous tissue binding organs |
- Form as part of an inflammatory process - Bind abdominal and pelvic organs together |
|
Ovarian Endometriomas |
Blood-filled cysts (chocolate cysts) on ovaries |
- Develop from endometrial cells spreading to ovaries - Cysts turn brown over time |
Possible symptoms:
- Severe pain in the pelvic area (often more noticeable during a period, when urinating, having bowel movements, or during intercourse). Most common symptom.
- Infertility
- Heavy bleeding during a period (or in between periods)
- Bloating
- Nausea
- Diarrhea/Constipation
- Fatigue
- Depression or anxiety
- Symptoms improve after menopause, though this is not always the case
- Some people with endometriosis do not experience any symptoms.
What is laparoscopic surgery?
Laparoscopic surgery, also known as keyhole surgery or minimally invasive surgery, is a procedure that allows surgeons access to the interior of the abdomen and pelvis without the need for large incisions. This approach relies on the use of a laparoscope, equipped with a light and camera, transmitting internal images to a screen.
Compared to traditional open surgery, laparoscopic procedures offer several advantages, including shorter hospital stays, faster recovery times, reduced post-operative pain and bleeding, and minimal scarring. This versatile technique is not only diagnostic but also is used for various surgical interventions, such as organ removal or obtaining tissue samples for biopsy.
Laparoscopy is most often used in the field of gynecology, gastroenterology, and urology. During the procedure, patients typically undergo general anesthesia. The surgeon makes small incisions (usually less than 1.5cm), through which the laparoscope, other surgical tools, and a tube for introducing gas into the abdomen are inserted. The insufflation of gas seperates the abdominal wall from organs, enhancing visualization on the video monitor.
Upon completion of the laparoscopic procedure, the gas is released, and the incisions are closed. While serious complications are rare, minor issues may affect 1-2% of patients postoperatively, such as infection, minor bleeding/bruising around incisions, and feelings of nausea and vomiting.
Serious complications, occurring in about 1 in every 1,000 cases, include damage to organs, major arteries, or complications related to the use of carbon dioxide, such as gas entering veins or arteries. Other rare but severe complications involve allergic reactions to anesthesia or the development of blood clots, potentially leading to deep vein thrombosis (DVT) and pulmonary embolism. In such cases, additional surgery may be necessary to address these complications.
What is robotic surgery?
Robotic surgery, also known as robot-assisted surgery, involves the use of small incisions, similar to laparoscopy. The most widely widely utilized Da Vinci robotic system consists of three main components:
- A surgeon’s console, where the surgeon sits and controls the robotic arms.
- A patient-side cart housing four robotic arms manipulated by the surgeon, with one designated for the camera and the others for various surgical instruments.
- A high-definition 3-D vision system, which enhances the surgeon's visibility during the procedure.
Though primarily associated with minimally invasive surgery, robotic surgery can also be applied to traditional open surgeries (my project focuses on the minimally invasive side). The advantages of this approach may include minimal tissue damage, reduced scarring, shorter hospital stays, and diminished pain and discomfort. The robotic system can offer enhanced precision and dexterity, as the robotic hands exhibit a greater range of motion and precision compared to human hands. The machine filters out any hand tremors from the surgeon, ensuring steadier hands for precise work. The longer reach of robotic arms allows access to areas that may be challenging with conventional laparoscopic instruments, enabling surgeons to perform procedures more effectively in confined spaces. The 3D visualization feature provides surgeons with a better view of the surgical field. The complication rate of robotic surgery seems to be similar to that of laparoscopic surgery.
Expert Opinion:
Dr. Liane Belland, MD, M.Sc, FRCSC
1. As a gynecologist, after you diagnose a patient with endometriosis, what do you often recommend as a treatment? When do you typically start considering surgical intervention?
2. In the event that surgery is used (for endo), what are some factors that influence the type of surgery chosen (standard laparoscopy, robotic surgery, laparotomy)?
3. In your practice, have you observed any qualitative differences (such as in postoperative recovery, effectiveness, pain management, or patient satisfaction) between laparoscopic and robotic surgery for endometriosis?
4. What areas of gynecological surgery would you like to see further researched?
6. Overall, which technique (laparoscopic surgery, robotic surgery) do you prefer to use for the treatment of endometriosis?
Results
Study characteristics and selection
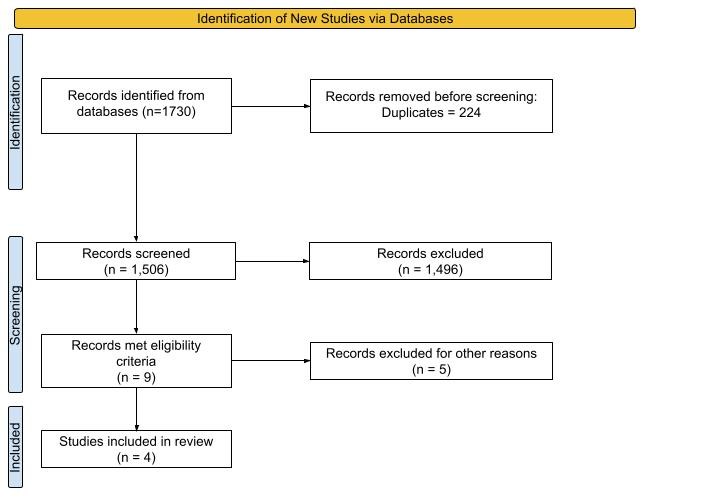
One thousand seven hundred thirty articles were identified. 224 duplicates were removed using Endnote. 1,496 articles were excluded, mainly for the following reasons: they did not directly compare only RAS to LPS, they did not focus on endometriosis, full-text versions could not be obtained, or they were not written in English. Nine articles met the inclusion criteria, however, 5 of these were included within a meta-analysis, and therefore three unique studies and a meta-analysis were included in the review. (Figure 1). The three individual studies were prospective cohort studies. The meta-analysis included four retrospective studies and one randomized controlled trial (RCT). A total of 1741 patients were identified in these selected studies, 959 from the LPS group and 782 from the RAS group.
The characteristics of the studies, including the name of the first author, year published, average age and BMI, and the study design, are shown in Table 1.

(Table 1)
Synthesis of the Results
All of the studies and the meta-analysis assessed the operating time of the procedures. The meta-analysis by Restaino, et al., reported a weighted mean difference of 0.54 min (95% CI, 0.37 to 0.70; p<0.0001) for operating time, with RAS requiring more time. The three prospective cohort studies (Ferrier et al., Raimondo et al., Le Gac et al.) reported similar results. Ferrier, et al. observed a mean operating time of 208 ± 90 mins for RAS, compared to 169 ± 81 mins for LPS (p = 0.01). Raimondo et al. reported a mean operating time of 207 ± 79 mins for RAS and 184 ± 214 mins for LPS (p = 0.171). Le Gac et al. showed a mean operating time of 221 ± 94 mins for RAS and 163 ± 83 mins for LPS (p=0.03). All of these results were reported with statistical significance. Hence, the operating time for RAS is longer than for LPS with statistical significance (p <0.05).
All studies also assessed the length of hospital stay (LOS) in both RAS and LPS. In the meta-analysis, the pooled estimate showed a weighted mean difference of 0.12 days but this was not significant. There was considerable variation within the prospective cohort studies, with no consistent trend and no significance. Raimondo et al. and Le Gac et al. showed that LOS was longer with RAS than LPS: 8 ± 4.4 days for RAS and 6.5 ± 2.6 days for LPS (Le Gac, et al.) and 8 ± 7 days for RAS and 6 ± 2 days for LPS (Raimondo, et al.). Contrastingly, Ferrier et al. showed that the LOS with LPS is slightly longer than RAS with 7.5 days ± 3.9 days for RAS and 7.8 ± 4.6 days for LPS. Overall, the results for the LOS for RAS compared to LPS are inconsistent, and no definitive conclusion can be drawn.
For blood loss, the meta-analysis reported no significant difference between RAS and LPS, with a WMD of 0.09mL. The individual cohort studies also had inconclusive results. Raimondo et al. and Le Gac et al. reported that blood loss (mL) with RAS is slightly higher than with LPS. For Raimondo et al., blood loss for RAS was 184 ± 214 mL compared to 144 ± 101 mL for LPS. Le Gac et al. had similar results; 130 ± 86 mL for RAS and 108 ± 99 mL for LPS. Ferrier et al., on the other hand, reported more blood loss with LPS than RAS, with 161 ± 141 mL for RAS and 188 ± 266 mL for LPS. None of these results had significance. Therefore, for blood loss, there is no clear trend, and the results are inconclusive.
Finally, operative complications were assessed as two sub-categories: intraoperative and postoperative complications. The meta-analysis reported a relative risk ratio (RR) of 1.27 for intraoperative complications in RAS compared to LPS; this was not significant. The prospective cohort studies reported mixed results with no significance. Raimondo et al. and Le Gac et al. both described a higher incidence of intraoperative complications in the RAS group compared to the LPS group. Raimondo et al. reported 1 patient (5% of patients) with intraoperative complication in the RAS group and 0 in the LPS group. Le Gac et al. reported 2 patients with intra-operative complications (9% of patients) in the RAS group and 1 in the LPS group (4% of patients). Contrary to these two studies, Ferrier et al. reported more intraoperative complications in the LPS group, with 2 cases in the RAS group (3.3% of patients) and 6 cases in the RAS group (9.8%).
For post-operative complications, the meta-analysis indicated an RR of 0.88 in RAS compared to LPS.; again, this was not significant. Raimondo et al. and Le Gac et al., contrary to the meta-analysis reported that RAS had a higher complication rate than LPS. Raimondo et al. reported 4 patients (18%) in the RAS group and 1 patient (5%) in the LPS group who experienced postoperative complications. For Le Gac et al., 6 patients (27%) in the RAS group experienced postoperative complications, while 4 patients (15%) in the LPS group experienced postoperative complications. Ferrier et al. had results similar to that of the meta-analysis, with LPS having a slightly larger incidence of postoperative complication in the LPS group with 21 reported cases (34.4%) compared to 20 reported cases (32.8%) in the RAS group. None of the results were statistically significant. Therefore, there is no clear or consistent correlation between the surgical technique used and the rate of perioperative complication.
Overall, the meta-analysis and related studies investigated key outcomes of robotic-assisted surgery (RAS) and laparoscopic surgery (LPS). Operating time was consistently longer for RAS (with statistical significance), while length of hospital stay (LOS), blood loss, and perioperative complication rates had inconclusive results between the two techniques.
Quality Assessments of Included Articles
|
The National Institutes of Health (NIH) quality assessment tool for observational cohort and cross-sectional studies Website: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools Comparison of perioperative outcomes between standard laparoscopic and robot-assisted approach in patients with rectosigmoid endometriosis - Raimondo, Diego |
|||
|
Major Components |
Response options |
||
|
1. Was the research question or objective in this paper clearly stated? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
2. Was the study population clearly specified and defined? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
3. Was the participation rate of eligible persons at least 50%? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
5. Was a sample size justification, power description, or variance and effect estimates provided? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
10. Was the exposure(s) assessed more than once over time? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
12. Were the outcome assessors blinded to the exposure status of participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
13. Was loss to follow-up after baseline 20% or less? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
Quality Rating |
Good |
Fair |
Poor |
|
C. The National Institutes of Health (NIH) quality assessment tool for observational cohort and cross-sectional studies Website: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools Comparison of robot‐assisted and conventional laparoscopy or colorectal surgery for endometriosis: A prospective cohort study - Ferrier, Clement |
|||
|
Major Components |
Response options |
||
|
1. Was the research question or objective in this paper clearly stated? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
2. Was the study population clearly specified and defined? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
3. Was the participation rate of eligible persons at least 50%? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
5. Was a sample size justification, power description, or variance and effect estimates provided? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
10. Was the exposure(s) assessed more than once over time? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
12. Were the outcome assessors blinded to the exposure status of participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
13. Was loss to follow-up after baseline 20% or less? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
Quality Rating |
Good |
Fair |
Poor |
|
C. The National Institutes of Health (NIH) quality assessment tool for observational cohort and cross-sectional studies Website: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools Comparison of robotic versus conventional laparoscopy for the treatment of colorectal endometriosis: Pilot study of an expert center - Le Gac, Marjolaine |
|||
|
Major Components |
Response options |
||
|
1. Was the research question or objective in this paper clearly stated? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
2. Was the study population clearly specified and defined? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
3. Was the participation rate of eligible persons at least 50%? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
5. Was a sample size justification, power description, or variance and effect estimates provided? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
10. Was the exposure(s) assessed more than once over time? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
12. Were the outcome assessors blinded to the exposure status of participants? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
13. Was loss to follow-up after baseline 20% or less? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
Quality Rating |
Good |
Fair |
Poor |
|
C. The National Institutes of Health (NIH) quality assessment tool of Systematic Reviews and Meta-Analyses Website: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools Robotic surgery vs laparoscopic surgery in patients with diagnosis of endometriosis: a systematic review and meta‐analysis - Restaino, Stefano |
|||
|
Major Components |
Response options |
||
|
1. Is the review based on a focused question that is adequately formulated and described? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
2. Were eligibility criteria for included and excluded studies predefined and specified? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
3. Did the literature search strategy use a comprehensive, systematic approach? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
4. Were titles, abstracts, and full-text articles dually and independently reviewed for inclusion and exclusion to minimize bias? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
5. Was the quality of each included study rated independently by two or more reviewers using a standard method to appraise its internal validity? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
6. Were the included studies listed along with important characteristics and results of each study? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
7. Was publication bias assessed? |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
8. Was heterogeneity assessed? (This question applies only to meta-analyses.) |
Yes |
No |
Cannot Determine/ Not Applicable/ Not Reported |
|
Quality Rating |
Good |
Fair |
Poor |
Discussion
Recently, the advent of robotic surgery has caught the attention of researchers, healthcare professionals, and patients. It has been professed to have the advantages of increased precision, dexterity, reduced blood loss, shorter hospital stays, less scarring, etc. However, our paper has demonstrated that RAS and LPS have similar outcomes in terms of blood loss, length of hospital stay, and rate of perioperative complications. In fact, the only statistically significant outcome was in favour of LPS, as LPS was reported to have a shorter operating time compared to RAS. Therefore, while RAS has been shown to have similar outcomes in safety (ie. blood loss and perioperative complications) and some measures of efficiency (ie. length of hospital stay) as LPS, it is not necessarily superior to LPS.
This review is one of few articles that examine the results of multiple studies and a meta-analysis to determine overall trends between RAS and LPS. We have summarized and synthesized the results of 3 prospective cohort studies, as well as a meta-analysis (which synthesized 3 retrospective studies and RCT). We have included both primary sources (the prospective studies) and a secondary source (the meta-analysis). However, some weaknesses need to be taken into account. One is the quality of the studies included. The studies were all prospective cohorts. The studies included in the meta-analysis were also of lower quality as they were retrospective, with only one RCT. Except for the RCT, these studies cannot make cause-and-effect claims and are not as controlled. In addition, no studies examined the long-term impacts of each surgical approach, such as pain relief or fertility outcomes. In addition, the screening process focused on searching electronic databases. While databases are important sources of information, books, conference papers, and other grey literature can also provide valuable information. In addition, many of the studies, including those in the meta-analysis, primarily focused on deep infiltrating endometriosis involving the colon or rectosigmoid, which makes it more difficult to draw conclusions for the treatment of other forms and stages of endometriosis.
Clinically, both robotic and standard laparoscopic surgery are acceptable techniques for the treatment of endometriosis in terms of blood loss, hospital stay, and complication rate. Robotic surgery, however, does have a longer operating time and that may be a factor in the decision between the use of robotic and standard laparoscopy.
In terms of future directions in this field, more well-designed RCTs are needed to examine the benefits and risks of RAS vs LPS. Additional studies with adequate follow-up would be extremely beneficial, allowing for a better understanding of the long-term effects of RAS compared to LPS. In addition, studies assessing other outcomes, such as patient satisfaction, fertility outcomes, and pain relief, would allow for a more holistic comparison between RAS and LPS.
Data
Raw Data
Operating Time
Restaino's Meta-Analysis Findings:
Revealed a weighted mean difference of 0.54 minutes (95% CI, 0.37 to 0.70; p < 0.0001) for operating time. RAS was found to require more time.
Prospective Cohort Studies:
Ferrier et al. - Observed a mean operating time of 208 ± 90 minutes for RAS, compared to 169 ± 81 minutes for LPS (p = 0.01).
Raimondo et al. - Reported a mean operating time of 207 ± 79 minutes for RAS and 184 ± 214 minutes for LPS (p = 0.171).
Le Gac et al. - Showed a mean operating time of 221 ± 94 minutes for RAS and 163 ± 83 minutes for LPS (p = 0.03).
Length of Hospital Stay
Restaino's Meta-Analysis Findings:
Pooled estimate from the meta-analysis revealed a weighted mean difference of 0.12 days for length of stay LOS between RAS and LPS, but it was not statistically significant.
Prospective Cohort Studies:
Raimondo et al. - Reported longer LOS with RAS (8 ± 7 days) compared to LPS (6 ± 2 days).
Le Gac et al. - Indicated longer LOS for RAS (8 ± 4.4 days) versus LPS (6.5 ± 2.6 days).
Ferrier et al. - Contrary to the other articles, showed a slightly longer LOS for LPS (7.8 ± 4.6 days) compared to RAS (7.5 ± 3.9 days).
Blood Loss
Restaino's Meta-Analysis Findings:
No significant difference in blood loss between RAS and LPS, with a Weighted Mean Difference (WMD) of 0.09 mL.
Prospective Cohort Studies:
Raimondo et al. - Reported slightly higher blood loss with RAS (184 ± 214 mL) compared to LPS (144 ± 101 mL).
Le Gac et al. - Indicated a similar trend with RAS showing slightly higher blood loss (130 ± 86 mL) than LPS (108 ± 99 mL).
Ferrier et al. - Again, in contrast with the other articles, reported higher blood loss with LPS (188 ± 266 mL) than RAS (161 ± 141 mL).
Operative Complications
Intraoperative Complications:
Restaino's Meta-Analysis Findings:
Reported a non-significant Relative Risk Ratio (RR) of 1.27 for intraoperative complications in RAS compared to LPS.
Prospective Cohort Studies:
Raimondo et al. - Higher incidence of intraoperative complications in RAS (5%) compared to LPS (0%).
Le Gac et al. - Noted a higher incidence of intraoperative complications in RAS (9%) versus LPS (4%).
Ferrier et al. - Differing results from the other papers, reporting more intraoperative complications in LPS (9.8%) compared to RAS (3.3%).
Postoperative Complications:
Restaino's Meta-Analysis Findings:
Indicated a non-significant RR of 0.88 for postoperative complications in RAS compared to LPS.
Prospective Cohort Studies:
Raimondo et al. - Higher postoperative complication rate in RAS (18%) compared to LPS (5%).
Le Gac et al. - Higher postoperative complication rate in RAS (27%) compared to LPS (15%).
Ferrier et al. - Similar to the meta-analysis, reported a higher incidence of postoperative complications in LPS (34.4%) compared to RAS (32.8%).
Note on graphs and tables: The inclusion of a meta-analysis and three prospective cohort studies as the sources has introduced a challenge in the creation of graphs. The meta-analysis provides a Weighted Mean Difference (WMD) between the two approaches, while the cohort studies present overall mean values, which makes it difficult to create a graph showing trends in the overall mean values for each approach (since the meta-analysis doesn’t include overall means). In addition, I did not want to oversimplify the results by calculating the overall mean of the studies included in the meta-analysis myself. Therefore, the data is presented in narrative form, rather than in tables/graphs.
Conclusion
Robotic surgery has not been shown, so far, to be superior to RAS in terms of operating time, blood loss, hospital stay, or rate of complication. However, it can be considered a valid option in place of LPS, though it does have a longer operating time. Clinically, while maintaining standard laparoscopy as the standard for the surgical treatment of endometriosis, consideration should still be given to robotic surgery. Further research into robotic-assisted surgery and laparoscopic surgery is needed, to hopefully enhance the well-being of every single patient living with endometriosis.
Citations
- A Guide To Understanding Endometriosis. Health. Accessed January 26, 2024. https://www.health.com/endometriosis-7152446
- asterdmhealthcare. What Is Robotic Endometriosis Surgery And What Are Its Advantages? www.asterdmhealthcare.com. https://www.asterdmhealthcare.com/health-library/what-is-robotic-endometriosis-surgery-and-what-are-its-advantages#:~:text=Robotic%20Endometriosis%20Surgery%20Benefits&text=Robotic%20endometriosis%20surgery%20scar%20is
- Bafort C, Beebeejaun Y, Tomassetti C, Bosteels J, Duffy JM. Laparoscopic surgery for endometriosis. Cochrane Database of Systematic Reviews. 2020;10(10). doi:https://doi.org/10.1002/14651858.cd011031.pub3
- Biz Care | Blog | Biz Care. www.biz-care.com. https://www.biz-care.com/blogs/nz/endometriosis-awareness-month-living-with-endometriosis
- Endometriosis - Symptoms and causes. Mayo Clinic. Published 2018. https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656#:~:text=Other%20symptoms%20include%20cramps%20that
- Endometriosis Surgery - Brigham and Women’s Hospital. Brighamandwomens.org. Published 2024. https://www.brighamandwomens.org/obgyn/infertility-reproductive-surgery/endometriosis/surgical-treatment-of-endometriosis-excision-and-destruction#:~:text=Excision%20of%20superficial%20peritoneal%20endometriosis
- Female Fertility Meeting | Google Slides & PPT. slidesgo.com. Accessed March 11, 2024. https://slidesgo.com/theme/female-fertility-meeting#search-women%26%23039%3Bs+health&position-6&results-131&rs=search&rs=search
- Ferrier C, Le Gac M, Kolanska K, et al. Comparison of robot‐assisted and conventional laparoscopy for colorectal surgery for endometriosis: A prospective cohort study. The International Journal of Medical Robotics and Computer Assisted Surgery. 2022;18(3). doi:https://doi.org/10.1002/rcs.2382
- How P-Values Help Us Test Hypotheses: Crash Course Statistics #21. www.youtube.com. Accessed January 26, 2024. https://www.youtube.com/watch?v=bf3egy7TQ2Q&list=PL8dPuuaLjXtNM_Y-bUAhblSAdWRnmBUcr&index=22&pp=iAQB
- John Hopkins Medicine. Endometriosis. John Hopkins Medicine. Published 2019. https://www.hopkinsmedicine.org/health/conditions-and-diseases/endometriosis
- Laparoscopic Surgery for Endometriosis | HealthLink BC. www.healthlinkbc.ca. https://www.healthlinkbc.ca/health-topics/laparoscopic-surgery-endometriosis#:~:text=Laparoscopy%20is%20used%20to%20examine
- Le Gac M, Ferrier C, Touboul C, et al. Comparison of robotic versus conventional laparoscopy for the treatment of colorectal endometriosis: Pilot study of an expert center. Journal of Gynecology Obstetrics and Human Reproduction. 2020;49(10):101885. doi:https://doi.org/10.1016/j.jogoh.2020.101885
- Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. Methodological Quality (risk of bias) Assessment Tools for Primary and Secondary Medical studies: What Are They and Which Is better? Military Medical Research. 2020;7(7). doi:https://doi.org/10.1186/s40779-020-00238-8
- Mathematical Thinking: Crash Course Statistics #2. www.youtube.com. Accessed January 26, 2024. https://www.youtube.com/watch?v=tN9Xl1AcSv8&list=PL8dPuuaLjXtNM_Y-bUAhblSAdWRnmBUcr&index=3&pp=iAQB
- Mayo Clinic. Robotic surgery - Mayo Clinic. Mayoclinic.org. Published May 6, 2022. https://www.mayoclinic.org/tests-procedures/robotic-surgery/about/pac-20394974
- National Institute of Health. Study Quality Assessment Tools | National Heart, Lung, and Blood Institute (NHLBI). Nih.gov. Published 2009. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- NHS Choices. Overview - Laparoscopy (keyhole surgery). NHS. Published 2019. https://www.nhs.uk/conditions/laparoscopy/
- P-Value Problems: Crash Course Statistics #22. www.youtube.com. Accessed January 26, 2024. https://www.youtube.com/watch?v=PPD8lER8ju4&list=PL8dPuuaLjXtNM_Y-bUAhblSAdWRnmBUcr&index=23&pp=iAQB
- Pautasso M. Ten simple rules for writing a literature review. Bourne PE, ed. PLoS Computational Biology. 2013;9(7). doi:https://doi.org/10.1371/journal.pcbi.1003149
- PRISMA. www.prisma-statement.org. https://www.prisma-statement.org/PRISMAStatement/Checklist
- Raimondo D, Alboni C, Orsini B, et al. Comparison of perioperative outcomes between standard laparoscopic and robot-assisted approach in patients with rectosigmoid endometriosis. Acta Obstetricia Et Gynecologica Scandinavica. 2021;100(9):1740-1746. doi:https://doi.org/10.1111/aogs.14170
- Restaino S, Mereu L, Finelli A, et al. Robotic surgery vs laparoscopic surgery in patients with diagnosis of endometriosis: a systematic review and meta-analysis. Journal of Robotic Surgery. 2020;14(5):687-694. doi:https://doi.org/10.1007/s11701-020-01061-y
- Rindos NB, Fulcher IR, Donnellan NM. Pain and Quality of Life after Laparoscopic Excision of Endometriosis. Journal of Minimally Invasive Gynecology. 2020;27(7):1610-1617.e1. doi:https://doi.org/10.1016/j.jmig.2020.03.013
- Saeed Pahlevan Sharif, Mura P, Sarah N.R. Wijesinghe. Systematic Reviews in Asia: Introducing the “PRISMA” Protocol to Tourism and Hospitality Scholars. Published online January 1, 2019:13-33. doi:https://doi.org/10.1007/978-981-13-2463-5_2
- Scientific Literature Review. https://www.dcu.ie/sites/default/files/students_learning/scientific_lit_review_workshop_ug.pdf
- The Himmelfarb Health Sciences Library. Meta-Analysis - Study Design 101. Gwu.edu. Published 2019. https://himmelfarb.gwu.edu/tutorials/studydesign101/metaanalyses.cfm
- UCLA health. What is Robotic Surgery? - Robotic Surgery | UCLA Health. www.uclahealth.org. https://www.uclahealth.org/medical-services/robotic-surgery/what-robotic-surgery
- Western Sydney University. Literature Review Purpose.; 2017. https://www.westernsydney.edu.au/__data/assets/pdf_file/0006/1254786/Literature_review_purpose.pdf
- What Is Statistics: Crash Course Statistics #1. www.youtube.com. Accessed January 26, 2024. https://www.youtube.com/watch?v=sxQaBpKfDRk&list=PL8dPuuaLjXtNM_Y-bUAhblSAdWRnmBUcr&index=2&pp=iAQB
- World Health Organization. Endometriosis. World Health Organization. Published March 24, 2023. https://www.who.int/news-room/fact-sheets/detail/endometriosis
- Yellow awareness ribbon and uterus icon vector isolated on a white... iStock. Published March 29, 2023. Accessed March 12, 2024. https://www.istockphoto.com/vector/march-is-endometriosis-awareness-month-vector-illustration-gm1477868090-506291961
Acknowledgement
Thank you to my mentor, Dr. Jenny Liao, M.D (Internal Medicine Resident at the University of Alberta) for giving me invaluable suggestions and tips during the process of writing my review. Thank you to Dr. Liane Belland MD M.Sc FRCSC (Gynecologist in the Bridgeland Advanced Gynecology Clinic and Clinical Assistant Professor at UofC) for answering my many questions about minimally invasive gynecology and endometriosis.
Thank you to Ms. Davis, our school's science fair coordinator.
Thank you to my parents for their support.

