Lower Limb Auxiliary Exoskeleton with Gait Management Feedback for Hypotonia
Grade 11
Presentation
Problem
Hypotonia is the most common condition affecting motor skills in newborns, with approximately 50% of children with Autism Spectrum Disorder experiencing hypotonia (Ming et al. 2007). Characterized by low muscle tone, hypotonia results in reduced resistance to movement at rest, leading to significant motor difficulties such as impaired walking ability. Current physiotherapy treatments primarily focus on muscle-strengthening exercises and the use of braces to assist with mobility (Physiopedia). While these interventions can improve movement to some extent, they do not necessarily address gait stability, often resulting in individuals developing unbalanced walking patterns.
An unbalanced gait presents challenges in everyday life, including difficulty navigating stairs, slopes, and uneven terrain. In a city like Calgary, where icy conditions persist for months, these challenges are exacerbated, posing serious safety risks to hypotonic individuals. Moreover, a long-term unbalanced gait can lead to other physical conditions. Studies have shown that "balance dysfunction and weight-bearing asymmetry" in walking gaits are highly correlated with anterior pelvic tilts (Kim et al. 2018). Such manifestations of muscle imbalances highlight the importance of developing a healthy walking gait and posture. While conventional mobility aids offer some assistance, they often lack the adaptability required to support proper posture and muscle engagement during movement. Given these limitations, there is a growing need for more advanced assistive technologies that not only facilitate walking but also promote a more balanced and stable gait.
As emerging mobility solutions, exoskeletons provide a more versatile and supportive alternative to traditional braces. With structural features such as a waist attachment for spinal and core stability, exoskeletons can offer more comprehensive support to individuals with hypotonia. This project aims to evaluate the efficacy of a lower limb auxiliary exoskeleton in assisting a hypotonic individual with walking while promoting a more balanced gait. By integrating gait management feedback, this study seeks to explore the potential of exoskeleton technology in improving both mobility and overall quality of life for individuals with hypotonia.
Problem: What is the efficacy of a lower limb auxiliary exoskeleton in helping to improve a hypotonic individual's unbalanced walking gait?
Market Size: Approximately 80,000 individuals (only accounting for autism-linked hypotonia in children)
"At least one million Canadians are autistic" (Autism Alliance of Canada 2024).
According to the 2021 Canadian population census, 6,012,795 individuals out of the 36,991,980 total population are children under the age of 14. This is roughly 1/6 of the population. Using this percentage to estimate the number of Canadian children that are autistic, that gives around 160,000. Using the statistics from Ming et al., it can be approximated that more than 80,000 children in Canada have hypotonia-marked autism. However, it is essential to note that the "exact incidence of hypotonia is difficult to determine because it is not a disease but a presenting feature of various diseases" (Madhok et al. 2022).
Method
This project aims to design an exoskeleton that 1) provides structural support to the lower limbs and 2) identifies the force exertion during gait. The second goal is significant because of the pivotal role that muscle engagement plays in fostering a balanced gait and preventing adverse outcomes such as poor posture and falling (Stotz et al., 2023). By identifying muscle contribution during walking, the exoskeleton should provide feedback to users, notifying them of incorrect gait patterns and postures.
The design objectives of this walking assistance exoskeleton can be broken down into its mechanical design objectives and system control objectives.
Mechanical Design Objectives: The exoskeleton’s frame is broken down into individual metal bars that act as the limbs, with rotational components that serve as the knee and hip joints. The rotational connection parts, powered by steering motors and gears, should have a reasonable degree of mobility corresponding to the user’s movements. The torso attachment should support the spinal cord when wrapped around the user's waist.
1: Main Skeletal Framework
- Composed of individual metal bars that serve as limb segments
- Incorporates rotational components designed to imitate the movement of the human lower body
2: Four DH-03X Large Torque Alloy Servos: the joints
- High-performance motors are powered by a 12V lithium-ion battery
- Placed at the hip and knee joint locations to mimic the movements of said joints
- 0.595 kg per Servo
- Torque: 180 kg.cm (≈17.65 Nm)
3: 3D Printed and Laser Cut Components
- Two pairs of C-shaped, 3D-printed elements that are securely affixed to each metal bar
- Based on user’s leg measurements
- Provides a snug fit and anchors the exoskeleton in place
- Reinforced with nylon straps
- System of three laser-cut acrylic components designed to govern the movements of the calf section
- Connected a Servo positioned above the knee on the calf metal bar
- 3D printed box to hold the control board
- All wirings are connected to this box
4: Torso Attachment
- Encircles the user’s waist to provide support for the spinal cord
- Designed to help with the user’s posture
5: Four 2*10*280 Springs
- One spring is attached to the calf bar of each leg
- Provides more supporting force when the knee bends
System Control Objectives: The steering motors, connected to an Arduino Nano Board, should move the rotational components according to a walking gait's range of mobility. The exoskeleton should also have some form of gait management feedback system to provide data based implications of the user's gait patterns and postures.
Electric Components
1: Arduino Nano Board: the central control module
- A powerful microcontroller with digital and analog pins compatible with an extensive array of sensors and other modules.
2: Force Sensitive Resistors (Pressure Sensors): for gait analysis
- Two sensors are placed at the heel and ball of the individual's foot
- Allows for the analysis of force exertion during gait
- Data helps to visually see an unbalance in the force exerted by each leg
Code Design
The exoskeleton is coded to mimic the natural gait of a healthy adult, which means that its degrees of motion follows the joint range of motion during a healthy adult's gait (Physiopedia).
Figure 1. Gait Cycle of a Healthy Adult (Physiopedia)
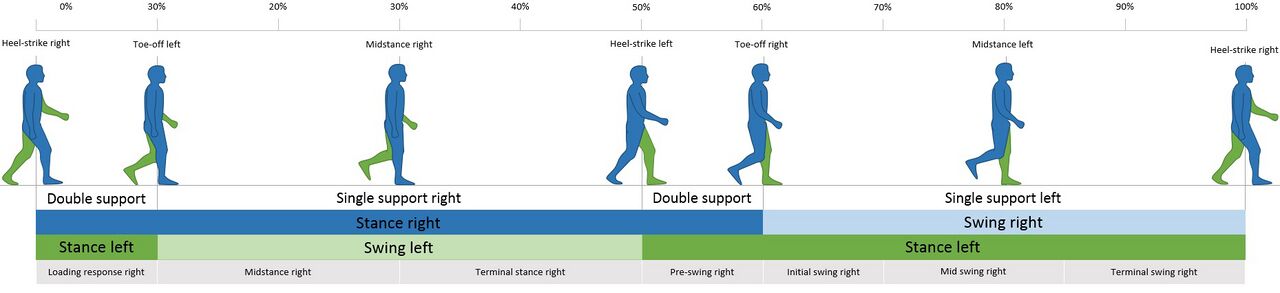
The exoskeleton also two other modes for stair ascent and descent. The angles for these codes were based on the data from a 2002 study (Riener et al. 2002).
Analysis
Results
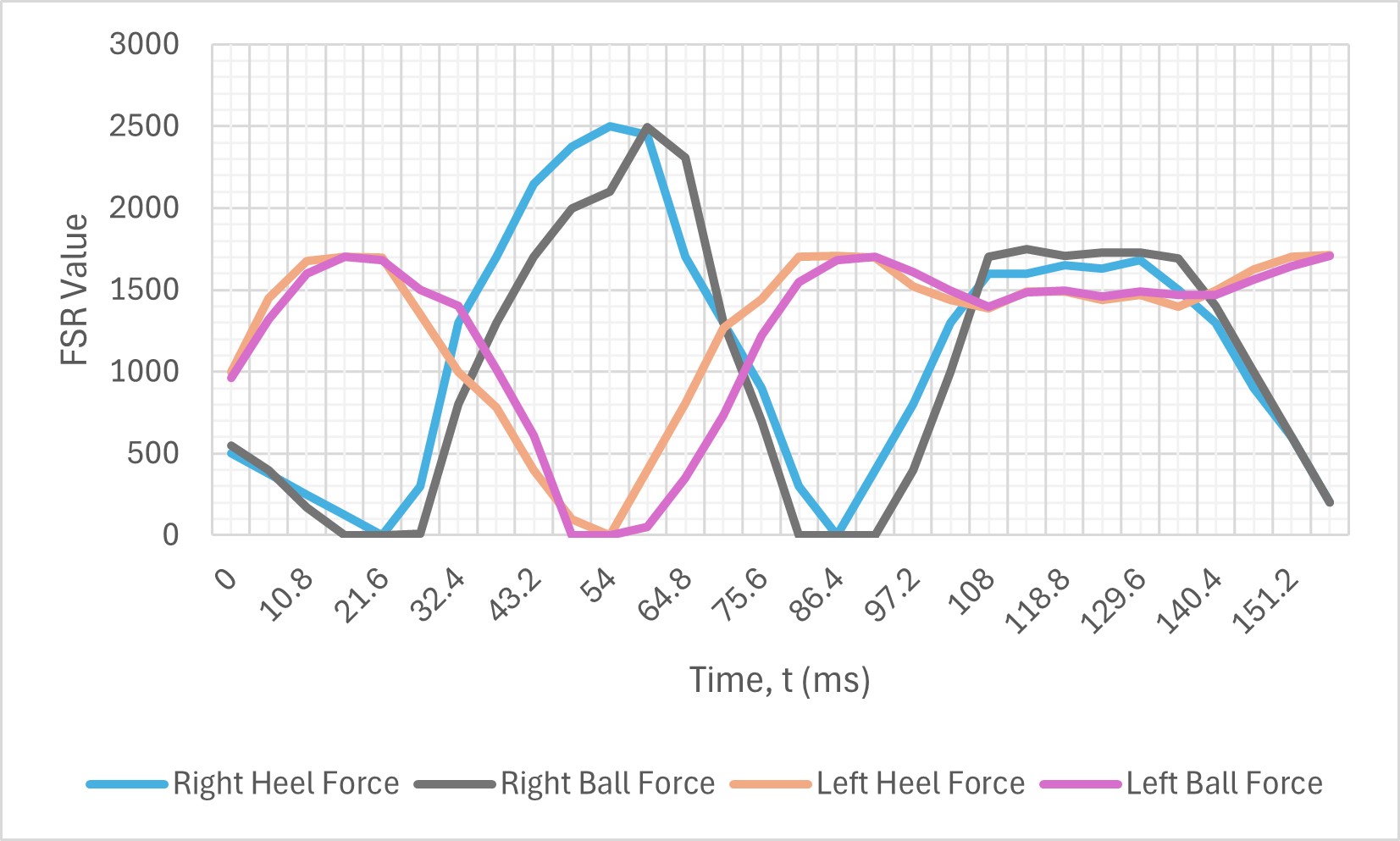
Analysis of whether force exertion is balanced or not during gait will be conducted through two perspectives:
1) Pressure on each foot
- The 4 FSRs recorded how much pressure was exerted on the heel and ball of each foot as the participant walked on flat ground without and with the exoskeleton.
2) Center of mass shift
- Videos of the participant walking on flat ground with and without the exoskeleton were taken. Then, Tracker, a free video analysis and modeling tool, tracked the shifting motion of the participant's center of mass (center of her back).
Graph 1. Pressure Detected by FSR on Feet Without Exoskeleton
Graph 2. Pressure Detected by FSR on Feet With Exoskeleton
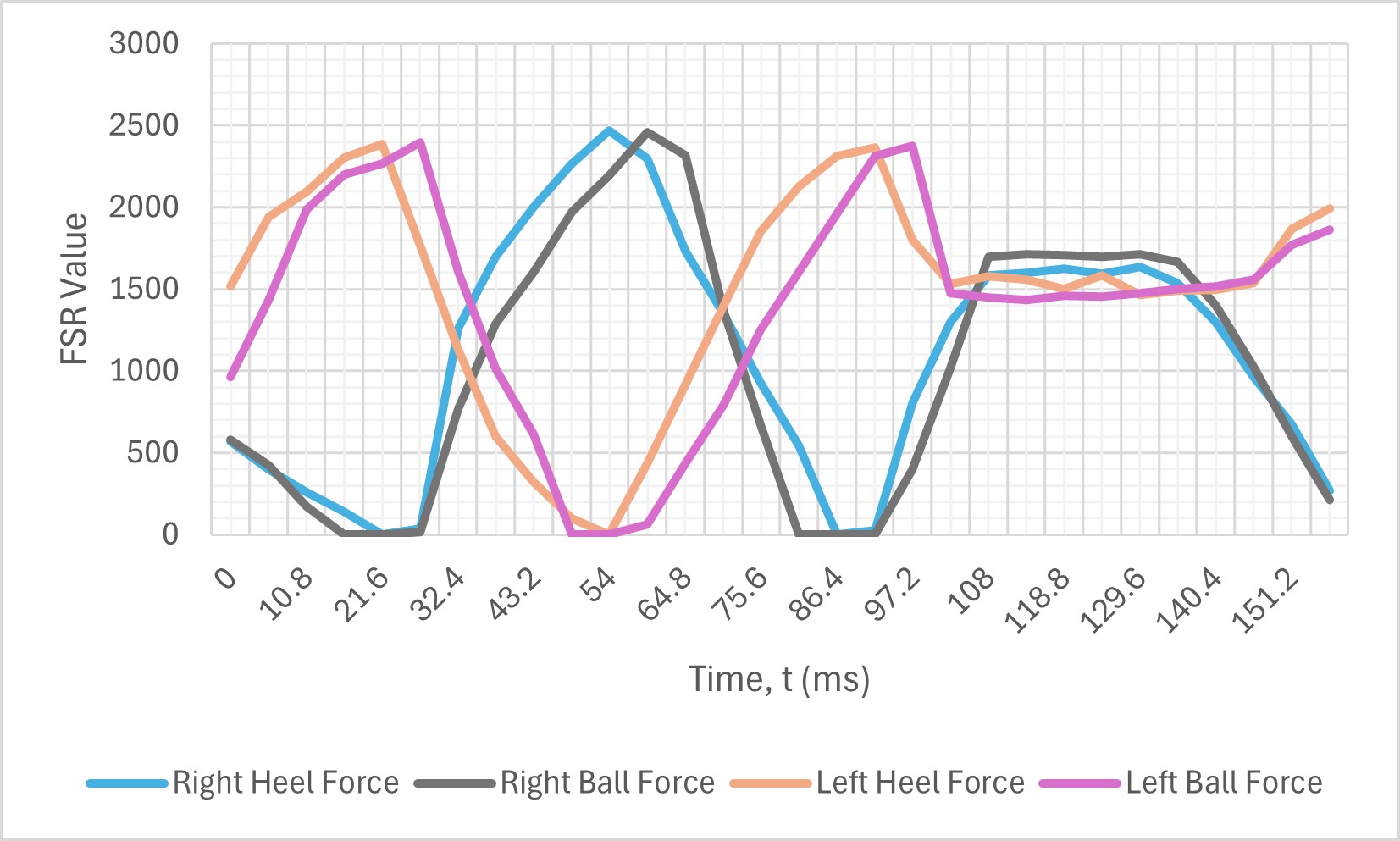
Graph 1 shows that, when walking normally without wearing the exoskeleton, the participant's pressure on her right foot is significantly higher than on her left foot. This discrepancy suggests that the participant's weight is mostly on her right leg, leading to an unbalanced walking gait. In contrast, the pressures detected in Graph 2 show a more minor difference between the force exertion of each leg when the participant walks with the exoskeleton on. The difference between the maximum pressure values in Graph 2 is 89.8% less than that of Graph 1. Therefore, the pressure analysis concludes that the exoskeleton effectively balances the pressure on each foot for an individual with hypotonia.
Graph 3. Center of Mass Shift When Walking Without Exoskeleton
![]()
Graph 4. Center of Mass Shift When Walking With Exoskeleton
![]()
Graph 3 shows how much the participant's center of mass deviates from the video's axial origin when she walks normally without the exoskeleton on. The imbalance of the participant's gait is especially apparent from seconds 1.0 to 2.0, where the center of mass shifts to the right of the origin significantly more than to the left (8 cm to the right, then 3 cm to the left). This occurrence aligns with the previous pressure data because a greater shift in center of mass to the right also indicates that the participant is placing most of her weight on her right leg when walking. The right and left shifts are comparably more balanced in Graph 4. For example, from seconds 3 to 5, the center of mass shift is roughly 10 cm to the right, 13 cm to the left, 11 cm to the right, and 9 cm to the left. The maximum difference in shift here is 3 cm, which is lower than the difference of 5 cm in Graph 3. Therefore, the analysis of the center of mass shift concludes that the exoskeleton is effective at balancing out weight shift, leading to a more balanced walking gait. However, it is important to note that her center of mass shift was greater while wearing the exoskeleton. This is because the exoskeleton adds more weight that she needs to shift from one leg to the other. This increased side-to-side movement in the upper body can be reduced by strengthening her core muscles. A stronger core will minimize movement in her upper body. This is a limitation of this project because the exoskeleton mainly focuses on balancing force exertion, and the results are most apparent in the lower body. Doing so neglects the upper body, so an improvement for this project would be to improve walking gait in hypotonic individuals holistically.
Conclusion
The results of this study demonstrate that the lower limb auxiliary exoskeleton effectively improves gait balance in an individual with hypotonia. By redistributing weight more evenly between the feet and balancing shifts in the center of mass, the exoskeleton enhances stability and promotes a more balanced walking pattern. These findings suggest that exoskeletons could serve as a viable form of physiotherapy for individuals with hypotonia in the future, providing mobility support and long-term benefits in improving gait mechanics. Unlike traditional braces, which focus primarily on structural support, this exoskeleton actively aids in gait correction, potentially reducing the risk of secondary issues such as joint pain or posture misalignment. Current forms of physiotherapy, such as muscle strengthening exercises, should be continued for individuals to gain a stronger core that will reduce excessive shifts in the center of mass.
Developing the exoskeleton presented several challenges, particularly in programming the Servos to replicate a natural walking motion. Fine-tuning the degrees of movement to match the gait of a healthy adult required extensive trial and error, highlighting the complexity of designing assistive technology that adapts to human biomechanics. Despite these difficulties, the exoskeleton successfully demonstrated its ability to improve balance, opening the door for further refinements. Future work could focus on expanding its functionality, such as assisting with walking up and down stairs, which is an essential but often difficult task for individuals with hypotonia. While a set of codes was developed for stair ascent and descent, it was not used during testing. The participant is currently only able to walk downstairs using one supporting leg, which does not match the exoskeleton's coding logic. A smooth transition from flat ground to stairs or slopes also requires the use of a laser sensor (or other modules) to identify the range in the terrain. This feature is currently a work in progress. Additionally, the technology could be adapted for different groups with mobility impairments, broadening its impact in rehabilitation and daily mobility assistance.
Citations
Canada, Autism Alliance Of, and Autism Alliance Of Canada. “Charting a Path to Inclusion: Realizing the Promise of Canada’s National Autism Strategy - Autism Alliance of Canada.” Autism Alliance of Canada - We guide autism policy in Canada by bringing research and community perspectives together., 9 Oct. 2024, autismalliance.ca/path-inclusion-national-autism-strategy.
Clément, Julien, et al. “Hip-Knee-Ankle (HKA) Angle Modification During Gait in Healthy Subjects.” Gait & Posture, vol. 72, May 2019, pp. 62–68. https://doi.org/10.1016/j.gaitpost.2019.05.025.
Government of Canada, Statistics Canada. Profile Table, Census Profile, 2021 Census of Population - Canada [Country]. 15 Nov. 2023, www12.statcan.gc.ca/census-recensement/2021/dp-pd/prof/details/page.cfm?LANG=E&GENDERlist=1,2,3&STATISTIClist=1&DGUIDlist=2021A000011124&HEADERlist=2,1&SearchText=Canada.
Kim, Myoung-Kwon, et al. “The Relationship Between Anterior Pelvic Tilt and Gait, Balance in Patient With Chronic Stroke.” Journal of Physical Therapy Science, vol. 30, no. 1, Jan. 2017, pp. 27–30. https://doi.org/10.1589/jpts.30.27.
Kuster, M., et al. “Kinematic and Kinetic Comparison of Downhill and Level Walking.” Clinical Biomechanics, vol. 10, no. 2, Mar. 1995, pp. 79–84. https://doi.org/10.1016/0268-0033(95)92043-l.
Lay, Andrea N., et al. “The Effects of Sloped Surfaces on Locomotion: A Kinematic and Kinetic Analysis.” Journal of Biomechanics, vol. 39, no. 9, June 2005, pp. 1621–28. https://doi.org/10.1016/j.jbiomech.2005.05.005.
Madhok, Sehajvir S., and Nadeem Shabbir. “Hypotonia.” StatPearls - NCBI Bookshelf, 12 Oct. 2022, www.ncbi.nlm.nih.gov/books/NBK562209.
Ming, Xue, et al. “Prevalence of Motor Impairment in Autism Spectrum Disorders.” Brain and Development, vol. 29, no. 9, May 2007, pp. 565–70. https://doi.org/10.1016/j.braindev.2007.03.002.
Park, Ga Young, et al. “Changes in Gait Parameters and Gait Variability in Young Adults During a Cognitive Task While Slope and Flat Walking.” Healthcare, vol. 8, no. 1, Feb. 2020, p. 30. https://doi.org/10.3390/healthcare8010030.
Physiopedia. “Hypotonia.” Physio-pedia, www.physio-pedia.com/Hypotonia.
---. “Joint Range of Motion During Gait.” Physio-pedia, www.physio-pedia.com/Joint_Range_of_Motion_During_Gait.
Ramakrishnan, H. K., and M. P. Kadaba. “On The Estimation of Joint Kinematics During Gait.” Journal of Biomechanics, vol. 24, no. 10, Jan. 1991, pp. 969–77. https://doi.org/10.1016/0021-9290(91)90175-m.
Riener, Robert, et al. “Stair Ascent and Descent at Different Inclinations.” Gait & Posture, vol. 15, no. 1, Feb. 2002, pp. 32–44. https://doi.org/10.1016/s0966-6362(01)00162-x.
Acknowledgement
Thank you to my mother for supporting my journey on this project and always being supportive when I needed to purchase materials for the project, even when I made mistakes when ordering different models.