The Alginate Solution: Dissolvable Stitches from Popping Boba
Grade 11
Presentation
Problem
Research Question:
Background:
Historical evidence for the widespread use of sutures for rudimentary surgery began around 3000 BCE (Carrington College, 2024) and often involved the use of plant-fiber based sutures and bone-needles. Fast forward to the 2nd century AD, evidence from Rome points to the first use of “catgut” sutures by Galen of Pergamon (Scheepers, 2014). Contrary to the name, this suture thread was often made from cattle, sheep, or goat intestines that have been dried and stretched.
A particular advantage for the use of catgut is the fact it is dissolvable and can be safely absorbed by the body after a wound is healed. Of course, catgut has become the forefather of contemporary synthetic dissolvable sutures made from biodegradable polymers like Polylactic acid (PLA) and Polyglycolide (PGA) which are also able to safely degrade in the body (Parthasarathy et al., 2017). Dissolvable stiches offer several benefits, including a reduced risk of infection, minimizing discomfort and inconveniences, as well as their biocompatibility (Universal Sutures, 2023).
These advantages are particularly pertinent to those in impoverished countries without much access to medical care. For one, the elimination of the need for suture removal for someone who already has limited access to healthcare increases the practicality and effectiveness of the sutures. This saves both the patient and the healthcare provider time and resources by allowing for greater access for the former and allow the latter to divert it to others. Additionally, reduced infection rates due to the lack of a second potential of exposure upon removing the stitches can also mean the difference between life and death for those who already have significantly reduced access to medical care.
And it truly is a matter of life or death for some. In Sierra Leone the maternal mortality ratio is 2 100 deaths per 100 000 live births, while in Ireland the ratio is 1 maternal death per 100 000 live births (Venkatapuram et al., 2013). What accounts for these huge discrepancies? Paul Farmer points to the lack of sutures, sterile drapes, and anesthesia is one of the many reasons for this outrageous maternal death ratio (2008). This sentiment is echoed by hundreds of other papers, all pointing to the lack of sutures as a primary cause of maternal death from complications arising from childbirth. These deaths can be prevented with increased access to sutures, particularly dissolvable sutures, especially in consideration of maternal deaths in which dissolvable stiches are often used.
Moreover, some of the reasons following the lack of use of these dissolvable sutures come from their higher cost. This is due to the high cost of the specialized synthetic materials used to derive the sutures as well as with the increase of cost that comes from its sophisticated chemical synthesis and processing. This drives the cost of dissolvable sutures up making this even more inaccessible for impoverished countries.
This investigation will be focusing on the development of a viable alternative to conventional dissolvable sutures. One of the major factors that contribute to healthcare inequalities when it comes to dissolvable sutures comes from the high cost of manufacturing contemporary dissolvable sutures and thus prevents this essential healthcare tool from being accessed by impoverished countries.
Elements that will designate a “viable” alternative will include as folllows; biocompatibility, cost-effectiveness, practicality (tensile strength, knot security, absorbability), and ease of access. As such, these elements will be investigated using research and experimentation to determine a viable alternative to dissolvable stitches.
Method
Suture Preparation
Determining a Viable Suture Material:
PLA and PGA polymers:
Gelatine:
When looking at biocompatible materials with the restriction that they can be dissolved by the body, it is pertinent to look at hydrogel materials such as gelatine. Gelatine possesses high biocompatibility, and it has been used in many slow-release drug delivery systems as well as in bandages and internal scaffolding for the body (Choi et al, 2021).
However, some of the issues that arise from collagen-based sutures is its ability to rehydrate and hydrate, which can decrease its overall stability. The collagen bonds are held together by hydrogen bonding from the water and thus, upon heating of the solution, the bonds have a high chance of breaking upon hydrolysis. This diminishes its overall effectiveness, as it is possible that upon contact with bodily fluids and high temperatures from the body the sutures may come undone or break. Gelatine has been shown to denature at around 37°C (Farrugia et al., 1999) which coincidentally is the same temperature of the human body. This means that the sutures are likely to dissolve at contact with the human body, rendering it impractical for dissolvable sutures.
For this reason, and based on previous study, sutures made from gelatine will not be considered. Thus, while gelatine is a very biocompatible material, it does not meet the standard for stability and will not be considered in this investigation.
Alginate:
Alginate or alginic acid is a naturally occurring polysaccharide derived from brown seaweed (Lee et al, 2012). Commercially, it has been used in the popular popping boba or popping pearls drink with the specification process. When exposed to a solution of calcium ions, the calcium ions replace the sodium ions, allowing for the alginate molecules to bind together and cross-link. This chemical reaction creates a thin membrane that encapsulates the liquid drop (Tsai et al., 2017).
Alginate is used in many biomedical applications, including wound dressing (by companies like AlgicellTM, SorbsanTM, etc.) and healing, drug delivery, and tissue engineering (Lee et al., 2012) and has been studied extensively as a biocompatible, non-toxic material. In addition, alginate is also non-immunogenic, meaning that the material has an antigen that will not trigger an immune response in the body (Raus et al., 2021). This is incredibly important, as rejection of the suture that triggers inflammation and the immune system can increase risk for infection as well as delay the healing process.
Regarding alginate’s stability, it has been shown that alginate microbeads are stable for over 6 weeks in several tissue locations with minimal change to volume and diameter of the beads (Moya et al., 2012). Additionally, due to alginate’s innate property of crosslinking in the presence calcium ions it can maintain its structural integrity with the calcium ions in the body. As calcium ions are essential for coagulation factors in blood clotting, and thus when the body senses injury, it will send calcium ions to the cite to facilitate wound healing. Alginate likewise uses calcium to crosslink itself, and the sutures can be strengthened by the body’s natural response of sending calcium ions to a wound site. Stabilty can also be increased with the integration of collagen molecules (from gelatine) or by adding stabilizers like Xantan Gum.
In addition, cost-effectiveness studies show that alginate is generally more cost effective. For example, with the use of alginate in silver dressing to treat pancreatic cancer, the cost of treatment was shown to cost almost $90 (USD) less than its component silver-zinc sulfasalazine cream (Chuangsuwanish et al., 2013). Its ease of access due to its use in food is also benefit, as it available in many commercial stores.
For these reasons alginate-based sutures will be the primary focus for this investigation as it meets the elements that designated a viable alternative including biocompatibility, cost-effectiveness, and ease of access.
Investigating the Properties of Alginate:
As the material for the sutures has been determined, additional investigations will discern the practicality of this solution between various concentrations of the alginate gel sutures. Various concentrations of the alginate solution will be prepared and dried to create the suture thread and tested for various indicators of practicality including tensile strength, knot security, and absorbability.
Safety Considerations:
Table 1: List of chemicals used and associated WHMIS and Hazards Identification
|
Chemical |
Nature of Hazard |
Symbols |
|
Sodium Alginate |
None |
N/A |
|
Calcium Chloride (CaCl2 (s) |
May form combustible dust concentration in air, eye irritation |
Warning |
First Aid:
Table 3: First Aid treatment for various routes of exposure for chemicals used
|
Route of Exposure |
Treatment |
Applicable Chemicals |
|
Inhalation |
Move to fresh air |
CaCl2 (s) |
|
Skin Contact |
Rinse with water for 15 minutes |
CaCl2 (s) |
|
Ingestion |
Do not induce vomiting. Get medical attention. |
CaCl2 (s) |
|
Eye Contact |
Rinse with water, remove contact lenses |
CaCl2 (s) |
Environmental and Disposal Considerations:
Dispose of Calcium chloride in household hazardous waste site at a designated Calgary fire station. Dispose of Sodium Alginate in a plastic bag and put into the garbage, do not pour down the drain.
Materials:
- 1x Sodium Alginate
- 1x Calcium Chloride
- 1x Distilled Water
- 2x Bowls
- 1x 3mL syringe
- 1x Blender
- 1x Stir Stick
- 1x Ruler
- 1x Balance
- 2x Beakers
Methodology for Suture Preparation:
Procedure:
- Measure out 5.0g of calcium chloride with the balance
- Dissolve the calcium chloride with 500mL of distilled water
- Measure out desired mass of sodium alginate
- Blend the sodium alginate in 500mL of distilled water
- Allow the sodium alginate solution to rest for at least 3 hours to remove any air bubbles from blender
- Take calcium chloride solution and place it in a long container
- Use the syringe to draw up the sodium alginate
- In a swift linear motion, place pressure on the syringe top and extrude the sodium alginate into the calcium chloride bath
- Wait about 5 minutes for the membrane to form. Rinse the polymer in a water bath
- Leave the polymer on a counter under a heat source for 2 hours or until the alginate has hardened
Variables:
Table 3: Independent, dependent and controlled variables including methodology and impact
|
Independent Variable |
Range and Scope |
Methodology |
|
Mass of Sodium Alginate (±0.1g) |
0.5 - 5.0 percent by mass by 0.5% increments |
Mass measured with a balance |
|
Dependent Variable |
Device, Precision |
|
|
Tensile Strength (±0.1g) |
|
|
|
Tensile Strength of Knots (±0.1g) |
|
|
|
Tensile Strength after Hydration (±0.1g) |
|
|
|
Controlled Variable |
Effect on Dependent variable |
Methodology |
|
Concentration of calcium chloride |
The concentration of calcium chloride is directly related crosslinking of alginate solution. If the concentration of calcium chloride is increased, then the alginate will become more crosslinked impacting it’s tensile strength. |
|
|
Type of syringe used |
Size of extrusion hole on the syringe impacts the diameter of alginate that is extruded. Thicker alginate extrusion is more prone to breakage and take longer to dry out and become the thread. |
|
|
Type of water |
Tap water (especially in Calgary) contains lots of minerals (including Calcium) which can gel the alginate before introduction to the bath. It also can change the concentration of calcium in the bath. |
|
|
Temperature of water of the calcium chloride bath |
The temperature of the bath has been shown to impact the formation of alginate (Indrani, 2013). This is because the crosslinking also depends on the energy of the surrounding system, and colder temperatures can slow the bonding of the alginate. |
|
|
Masses used for Force calculation |
Variations in the size and shape of the masses can influence gravitational pull and thus it’s mass, ultimately impacting the force calculation. |
|
|
Type of Knot |
Different knot types can place pressure on the threads, also impacting the breaking point. |
|
|
Method of extruding the sodium alginate |
Kinks or variations of the extruded alginate polymer can create breaking/weak points in the thread. |
|
|
Time in the calcium chloride bath |
More time in the bath allows for more access to the calcium ions and thus more crosslinking of the alginate |
|
|
Time in water bath for rehydration |
A longer time in the rehydration can impact how much water is able to renter into the polymer, thus impacting its strength |
|
|
Time drying on counter |
A longer drying time can influence how brittle or soft the alginate sutures become. |
|
Analysis
Raw Data:
|
Mass of Sodium Alginate (±0.1g) |
Qualitative Observations |
|
2.5 |
Solution is slightly more viscus than water |
|
5.0 |
More viscous than previous solution, slight tinge of color and cloudiness |
|
7.5 |
Similar to previous solution, more of a tinge of color and cloudiness |
|
10.0 |
Significantly more viscous, little flow, cloudier and greyer colored |
|
12.5 |
Glue-like viscosity, traps large air bubbles, cloudier and greyer |
|
15.0 |
Thick glue-like viscosity, traps small air bubbles, cloudier and greyer. Sticky and cannot flow off stir stick |
|
17.2 |
Thick slime-like viscosity, traps small air bubbles, cloudier and greyer. Sticky and cannot flow off stir stick |
|
20.0 |
Slime-like consistency, breaks rather than flows, grey and quite cloudy, traps small and large air bubbles |
Table 5: Number of Quarters alginate suture held before breaking point over three trials for simple tensile strength, tensile strength with a knot, and rehydrated tensile strength
|
Mass of Sodium Alginate (±0.1g) |
Tensile Strength (Number of Quarters) |
Tensile Strength with Knot Number of Quarters |
Tensile Strength once Rehydrated (Number of Quarters) |
||||||
|
|
Trial 1 |
Trial 2 |
Trial 3 |
Trial 1 |
Trial 2 |
Trial 3 |
Trial 1 |
Trial 2 |
Trial |
|
2.5 |
9 |
8 |
8 |
3 |
9 |
5 |
5 |
6 |
4 |
|
5.0 |
14 |
25 |
31 |
20 |
36 |
38 |
39 |
22 |
35 |
|
7.5 |
34 |
13 |
23 |
25 |
32 |
17 |
25 |
27 |
30 |
|
10.0 |
13 |
7 |
12 |
5 |
11 |
13 |
10 |
6 |
14 |
|
12.5 |
9 |
11 |
8 |
7 |
4 |
4 |
3 |
2 |
5 |
|
15.0 |
4 |
2 |
5 |
2 |
1 |
0 |
5 |
2 |
0 |
|
17.2 |
3 |
3 |
3 |
1 |
0 |
0 |
2 |
2 |
1 |
|
20.0 |
1 |
0 |
0 |
0 |
0 |
0 |
1 |
0 |
3 |
Processed Data:
NOTE: SEE ATTACHED DOCUMENT FOR FORMATTED CALCULATIONS AND FORMULAS
Percent Mass For sodium alginate Solution for 2.5g of sodium alginate:
(Solute Mass / Solution Mass) × 100%= 2.5g / 500g × 100%=0.5%
Uncertainty:
RUsolute= 0.1g/2.5g=0.04
RUsolution= 25 g/500 g = 0.05
AU=(0.04+0.05)0.5% = 0.045%
∴Percent Mass = 0.50 ± 0.05 %
Sample Calculation for average number of coins and mass for 2.5g of sodium alginate standard tensile strength:
=(9+8+8)/3=8.333… coins × 4.5g=37.5g
Uncertainty:
RUmass= 0.1g/4.5g=0.0222…
AU=0.0222…/37.5g=0.833…g
∴Mass of Coins= 37.5 ± 0.8 g
Sample Calculation for Force withstood by 2.5g of sodium alginate standard tensile strength:
F=ma=(0.0375 kg)(9.81m/s2) = 0.368 N
Uncertainty:
*Note: gravitational acceleration is a referenced value and therefore as an unknown uncertainty that cannot be tabulated below.
RUmass= 0.8g/37.5g=0.0213…
AU=0.0213…/0.368N=0.007850…N
∴Mass of Coins= 0.368 ± 0.008 N
Table 6: Mass alginate suture held before breaking point averaging three trials for simple tensile strength, tensile strength with a knot, and rehydrated tensile strength
|
Percent by Mass Alginate (±0.05 %) |
Tensile Strength (±0.8 g |
Tensile Strength with Knot (±0.8 g |
Tensile Strength Rehydrated (±0.8 g |
|
0.50 |
37.5 |
25.5 |
22.5 |
|
1.00 |
105.0 |
141.0 |
144.0 |
|
1.50 |
105.0 |
111.0 |
123.0 |
|
2.00 |
48.0 |
43.5 |
45.0 |
|
2.50 |
42.0 |
22.5 |
15.0 |
|
3.00 |
16.5 |
4.5 |
10.5 |
|
3.50 |
13.5 |
1.5 |
7.5 |
|
4.00 |
1.50 |
0.0 |
6.0 |
Table 7: Force alginate suture held before breaking point for simple tensile strength, tensile strength with a knot, and rehydrated tensile strength
|
Percent by Mass Alginate (±0.05 %) |
Tensile Strength (±0.008 N |
Tensile Strength with Knot (±0.008 N |
Tensile Strength Rehydrated (±0.008 N |
|
0.50 |
0.368 |
0.250 |
0.221 |
|
1.00 |
1.030 |
1.383 |
1.412 |
|
1.50 |
1.030 |
1.089 |
1.206 |
|
2.00 |
0.471 |
0.426 |
0.441 |
|
2.50 |
0.412 |
0.221 |
0.147 |
|
3.00 |
0.162 |
0.044 |
0.103 |
|
3.50 |
0.132 |
0.015 |
0.075 |
|
4.00 |
0.015 |
0.000 |
0.059 |
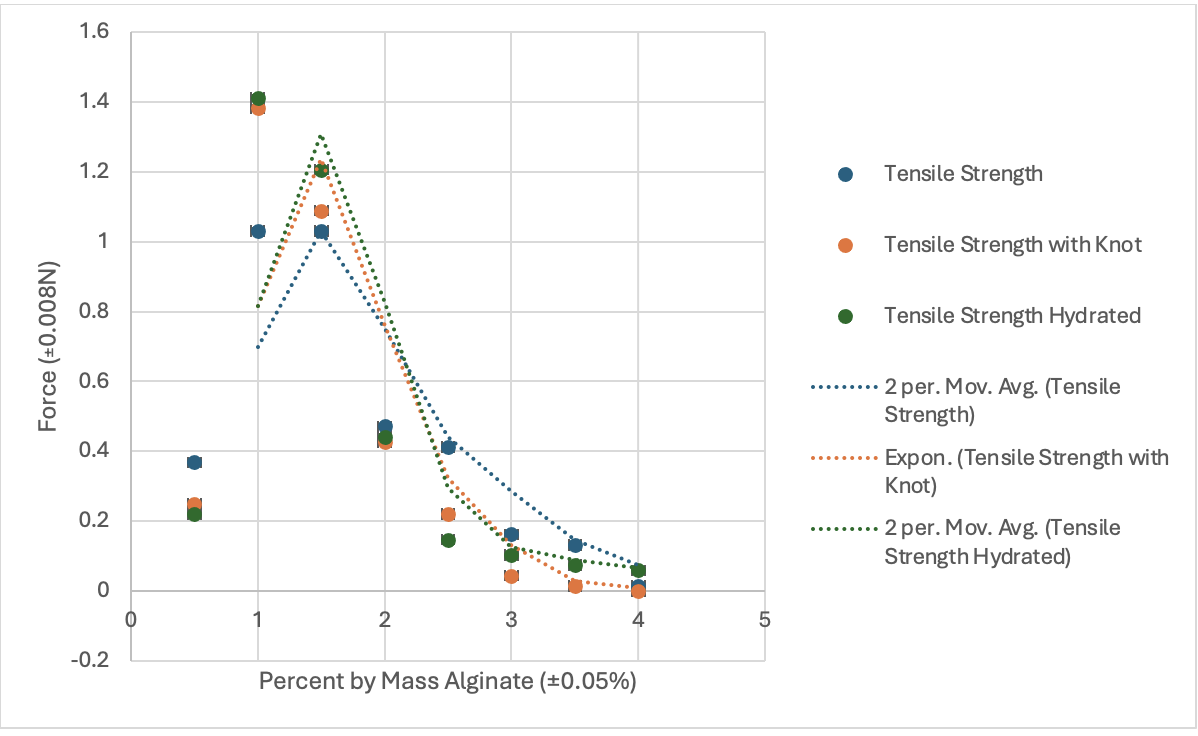
Figure 1: Force as a function of Percent by Mass alginate suture solution before breaking point for simple tensile strength, tensile strength with a knot, and rehydrated tensile strength.
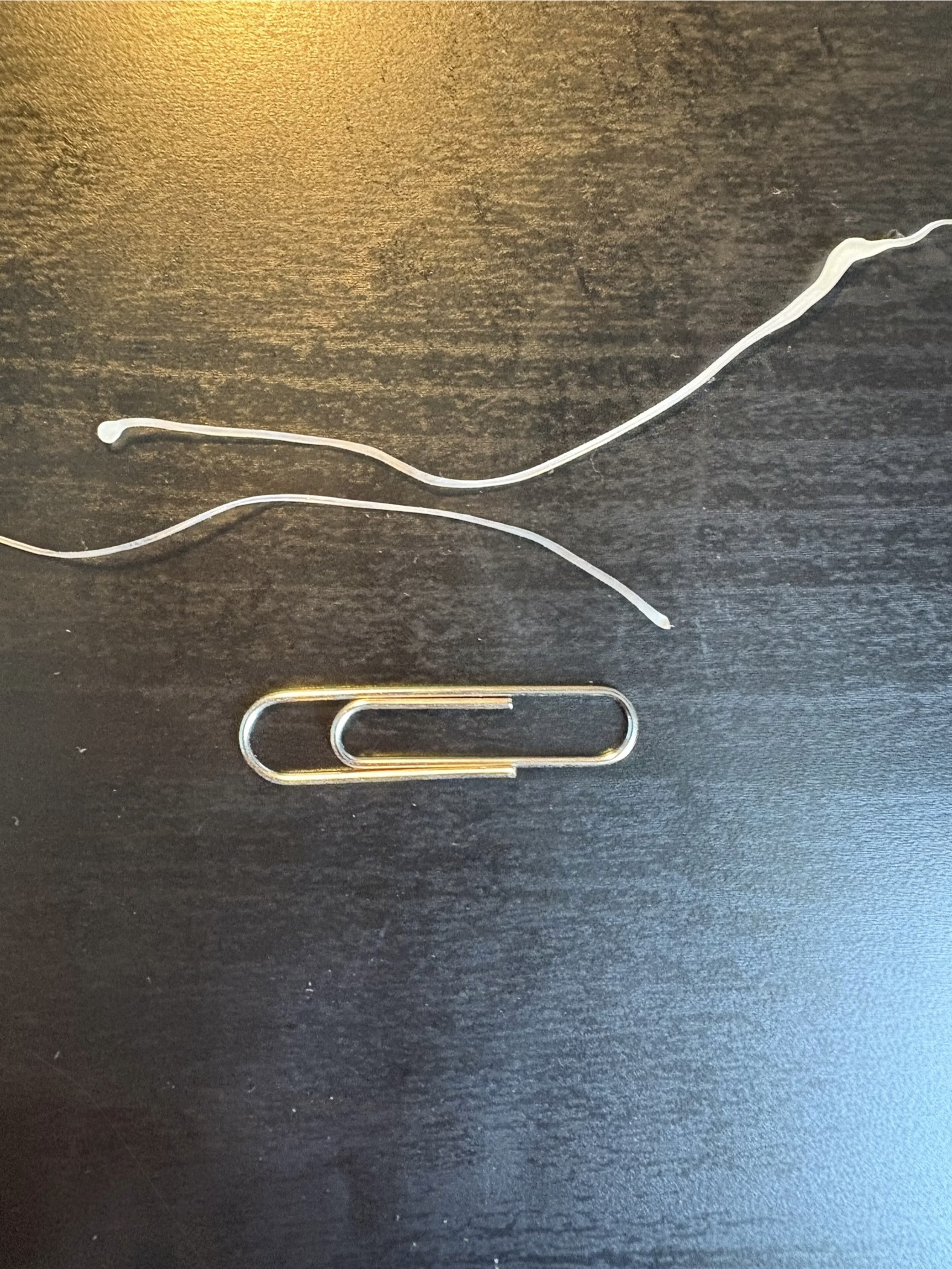 Figure 2: Side by side comparision of 1-2% by mass alginate in reference to a standard paperclip.
Figure 2: Side by side comparision of 1-2% by mass alginate in reference to a standard paperclip.
Conclusion
Conclusion:
The main purpose of this project was to investigate ways to lower healthcare inequalities across the globe by developing a viable alternative to dissolvable sutures. Too many countries face issues regarding their inability to access the crucial medication and tools that is needed to save lives. Particular to sutures, a lack of accessibility to sanitary, effective, and inexpensive dissolvable sutures can prevent mothers from receiving life-saving cesarean operations that could prevent maternal mortality. Using research and some at-home-experimentation, an alternative has been developed that could change this narrative, allowing for greater access to this unalienable right.
To find a viable alternative to these dissolvable sutures’ biocompatibility, cost-effectiveness, practicality (tensile strength, knot security, absorbability), and ease of access were all assessed. The following briefly analyzes the findings from these investigations:
Biocompatibility was difficult to experiment on directly, so research was imparted to draw conclusions to the effectiveness and safety of alginate in the human body. From this research, seen in the background and methodology, it was discovered that alginate possesses significant non-toxic, biocompatible, and non-immunogenic properties. Moreover, alginate’s current use in tissue scaffolding demonstrates its biodegradability within the human body in addition to its biocompatibility. Thus, alginate meets the biocompatibility and biodegradability aspects of this alternative.
As for cost-effectiveness, this can be determined by Chuangsuwanish’s 2013 study which investigated the cost effectiveness of sodium alginate as a drug delivery system for cancer. In addition, considering its relatively inexpensive price online or in grocery stores, it could certainly be mass produced for a very little cost. In comparison to PGA gut dissolvable sutures that run for about $225 for a box of 12 (a little under $20 per unit), the alginate sutures could cost a fraction of that price as they don’t require complicated manufacturing processes. Alginate sutures can also be made a lot more quickly in a matter of minutes, while typical absorbable sutures take around 64 hours to manufacture (Yanistsky et al., 1981).
With practicality, specifically focusing on the thread’s tensile strength and knot security, it can be discerned from Figure 1 that alginate concentrations from about 1-2% had the best tensile strength across all categories. This means that the suture thread will be able to stand about 1 Newton of force. While this tensile strength is not suited for sutures on the surface of the skin or on areas that may exert more force, it is well suited for cutaneous and soft tissue surgery, like the ones done in C-sections. Thus, it’s practicality and suitability as a dissolvable suture alternative is there. Furthermore, more research and experimentation could be done to find ways to increase the tensile strength, perhaps by adding collagen to strengthen the sutures or otherwise.
Finally, regarding ease of access. Considering the creation of these sutures is incredibly easy as well as possible with household ingredients it can be concluded that these sutures are relatively easy to access overall. This ensures that it would be a viable alternative to those in impoverished countries as they would likely be able to manufacture the material themselves.
Limitations and Further Study:
|
Limitation |
Impact on Investigation |
Further Study/Improvement |
|
Measurement of Tensile Strength |
The measurement of tensile strength of the sutures using masses may have been inaccurate as one is calculating indirectly. In addition, the set up for seeing the mass that the thread sometimes caused the thread to slip and come loose, perhaps creating new breaks in the suture thread. |
Using a force meter or a tensile strength device to get exact readings rather than calculated ones. |
|
Materials Used (combine to be stronger) |
Only alginate was investigated, however, many commercial products have mixtures of different materials, thus not all possibilities for alginate as a suture were explored which may have led to a lower force measurement than expected. |
Continue research and experiments using collagen or other biocompatible materials to make the alginate stronger and more stable (without becoming brittle) and increase the tensile strength of the sutures. |
|
Kinks and unevenness in extruded alginate suture |
Unevenness in the surface of the alginate extrusions created weak spots that often broke when doing tensile strength tests. |
Continue research on increasing the viscosity of the alginate (without making it more brittle). Better methods of extruding the alginate, potentially have it remotely controlled to always have an even pressure and speed and reduce kinks. |
Citations
References
Carrington College Blog. (2024, May 15). The Evolution of Surgical Sutures: From Traditional to Absorbable and Beyond. Carrington College. Retrieved 2025, from https://carrington.edu/blog/the-evolution-of-surgical-sutures-from-traditional-to-absorbable-and-beyond/
Choi, D., Choi, K., Park, S. J., Kim, Y.-J., Chung, S., & Kim, C.-H. (2021, October 27). Suture Fiber Reinforcement of a 3D Printed Gelatin Scaffold for Its Potential Application in Soft Tissue Engineering. National Library of Medicine. Retrieved 2025, from https://pubmed.ncbi.nlm.nih.gov/34769034/
Chuangusanich, A., Chortakarnkji, P., & Kangwanpoom, J. (2013, September 13). Cost-effectiveness analysis in comparing alginate silver dressing with silver zinc sulfadiazine cream in the treatment of pressure ulcers. National Library of Medicine. Retrieved 2025, from https://pubmed.ncbi.nlm.nih.gov/24086815/
ETHICON. (n.d.). BASIC KNOTS. ETHICON. Retrieved 2025, from https://www.kumc.edu/documents/plasticsurg/Surgery-Knot_Tying_.pdf
Instructables. (n.d.). Spherification (Direct Method). Instructables. Retrieved 2025, from https://www.instructables.com/Spherification-Direct-Method/
Juarez, G., Spasojevic, M., Faas, M., & Vos, P. (2014, August 6). Immunological and Technical Considerations in Application of Alginate-Based Microencapsulation Systems. National Library of Medicine. Retrieved 2025, from https://pmc.ncbi.nlm.nih.gov/articles/PMC4123607/
Lee, K., & Mooney, D. (2013, January 1). Alginate: properties and biomedical applications. National Library of Medicine. Retrieved 2025, from https://pmc.ncbi.nlm.nih.gov/articles/PMC3223967/
Nunamaker, E., Purcell, E., & Kipe, D. (2007, November 3). In vivo stability and biocompatibility of implanted calcium alginate disks. Wiley InterScience. Retrieved 2025, from https://deepblue.lib.umich.edu/bitstream/handle/2027.42/57402/31275_ftp.pdf;jsessionid=81E86A5EACED0E2414F052EBFAA80F7A?sequence=1
Parthasarathy, M., & John, A. A. (2023). 9 - Tribology of biodegradable polymeric systems. 9 - Tribology of biodegradable polymeric systems. Retrieved 2025, from https://www.sciencedirect.com/science/article/abs/pii/B9780323907484000169
Rather, J., Akhter, N., Ashraf, Q., Mir, S., Majid, D., Barba, F., Khaneghah, A., & Dar, B. (2022, Ddecember). A comprehensive review on gelatin: Understanding impact of the sources, extraction methods, and modifications on potential packaging applications. Food Packaging and Shelf Life. Retrieved 2025, from https://www.sciencedirect.com/science/article/pii/S2214289422001375
Raus, R., Nawawi, W., & Nasaruddin, R. (2021, May). Alginate and alginate composites for biomedical applications. Asian Journal of Pharmaceutical Sciences. Retrieved 2025, from https://www.sciencedirect.com/science/article/pii/S1818087620306437#:~:text=Although%20alginate%20is%20considered%20as,high%20G%20content%20%5B27%5D.
Samui, A., & Kanai, T. (2019). Polyhydroxyalkanoates based copolymers. International Journal of Biological Macromolecules. Retrieved 2025, from https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/ring-opening-polymerization#:~:text=However%2C%20the%20drawbacks%20of%20ring,the%20toxicity%20of%20catalysts%20etc.
Scheepers, A. (2014, December 3). https://theapprenticedoctor.com/historical-glimpse-suturing/. Apprentice Corporation. Retrieved 2025, from https://theapprenticedoctor.com/historical-glimpse-suturing/
Schmitt, F. (1971, March). A new absorbable suture. Wiley Online Library. Retrieved 2025, from https://doi.org/10.1002/jbm.820050207
Tsai, F.-H., Chiang, P.-Y., Kitamura, Y., Kokawa, M., & Islam, M. (2017, January). Producing liquid-core hydrogel beads by reverse spherification: Effect of secondary gelation on physical properties and release characteristics. Food Hydrocolloids. Retrieved 2025, from https://www.sciencedirect.com/science/article/abs/pii/S0268005X16302909
UNISUR. (2023, May 25). Absorbable Sutures Benefits. Improving Wound Healing And Patient Experience. Retrieved 2025, from https://www.universalsutures.com/sutures/benefits-of-absorbable-sutures/Absorbable Sutures Benefits
Acknowledgement
First, I would also like to thank my science teacher for his support and mentorship throughout this process. I also would like to thank my family for buying me all of my materials and putting up with the many alginate polymers that I've made (and left lying around) over the past few months!

