Can You Fake It? A study on the neuro-bio-psycho-social causes and effects for the prevention and identifications of suicide in adolescents.
Natania Varghese
Grade 9
Presentation
Problem
The problem of adolescent suicide represents a multifaceted societal concern with profound implications for the well-being of individuals, families, and communities. In the context of my research project, this issue is particularly urgent due to the complex interplay of factors, especially within the neuro-bio-psycho-social model, contributing to suicidal behaviours among adolescents.
Adolescence is a critical developmental period marked by significant changes. For many young people, navigating this transition can be hard and hectic, as they grapple with identity questioning and formation, peer relationships, academic pressures, and familial expectations. Additionally, adolescents may face unique stressors, as a result of our generation's advances, such as cyberbullying, social media pressures, and societal stigma surrounding mental health issues.
Within this context, the emergence of suicidal ideation and behaviours among adolescents is often a manifestation of underlying psychological distress, mental health disorders, or unresolved trauma. Biological factors, including genetic predispositions and neurochemical imbalances, can also contribute to increased vulnerability to suicidal ideation and actions. Furthermore, social determinants such as family dynamics, socioeconomic status, access to mental health care, and cultural attitudes towards suicide play significant roles in shaping an individual's risk profile.
The "Can You Fake It" project recognizes the urgency of addressing and identifying this problem by employing a comprehensive, multidisciplinary approach to the detection of suicide, By integrating insights from neuroscience, biology, psychology, and sociology, the research aims to uncover the intricate mechanisms and markers underlying suicidal behaviours in adolescents. Specifically, the project seeks to identify biomarkers, neural correlates, psychological profiles, and social dynamics that may serve as indicators of suicide risk.
Through this in-depth analysis, the project endeavours to develop innovative strategies for the prevention and early identification of adolescent suicide. By understanding the complex interplay of biological, psychological, and social factors, I hope to inform the development of targeted interventions and support systems tailored to the unique needs of at-risk adolescents.
Ultimately, addressing the problem of adolescent suicide is not only a matter of individual well-being but also a collective responsibility to nurture resilient, mentally healthy communities. By advancing our understanding of this complex issue and developing evidence-based interventions, the "Can You Fake It" project aims to contribute to a society where young people can thrive emotionally, socially, and academically.
Method
1. Social Media Datamining
- Reddit and Quora are online platforms where individuals ask questions and engage in discussions on various topics. For my project, I utilized these platforms to gather anecdotal information and opinions related to my specific questions.
- Methodologically, I searched for relevant subreddits on Reddit or topics on Quora that were closely aligned with my research questions.
- I used specific keywords or phrases related to my topic to find threads or questions where users had shared their experiences, opinions, or knowledge.
- Data collection from Reddit and Quora involved reading through discussions, comments, and answers to compile qualitative information that could provide insights into my research questions.
2. Research Studies
- Utilizing research studies involves accessing scholarly articles, journals, and academic publications relevant to my topic.
- I conducted searches on academic databases such as PubMed, Google Scholar, or specific journal databases to find peer-reviewed studies related to my research questions.
- The selection of research studies involved criteria such as publication date, relevance to my topic, methodology, sample size, and credibility of the authors and journals.
- Data collection from research studies involved reading through the literature to extract relevant findings, statistics, methodologies, and conclusions.
- I cited these studies to support arguments, provide evidence, and contextualize my findings within the existing body of scientific knowledge.
3. Analysis and Synthesis.
- - After collecting data from Reddit, Quora, and research studies, I engaged in analysis and synthesis to organize and interpret the information gathered.
- The analysis involved identifying common themes, trends, or patterns across the data sources.
- Synthesis entails integrating findings from different sources to develop a comprehensive understanding of the topic.
- I compared and contrasted perspectives from Reddit and Quora with findings from research studies, highlighting areas of agreement or divergence.
- Through analysis and synthesis, I aimed to derive meaningful insights, draw conclusions, and address my research questions and hypotheses.
By merging data gathered from Reddit, Quora, and rigorous research studies, I utilized a multi-layered approach to data collection, encompassing both qualitative and quantitative sources. This comprehensive methodology empowered me to investigate my research questions from diverse perspectives, enabling a nuanced understanding of the topic. By triangulating information from different sources, I could cross-validate findings, enhancing the robustness and reliability of my conclusions. This integrated approach not only enriched my analysis but also offered insights that might have been overlooked with a single-source method. Ultimately, this approach strengthens the validity of my research findings and contributes to a more holistic understanding of the subject matter.
Research
Background Information
- Improving suicide prevention efforts requires objective prediction of suicide risk and identification of effective treatments, extending beyond major psychiatric illnesses.
- Currently, clinical predictors are limited, and no established biomarkers exist.
- Despite the heterogeneous nature of suicidal behaviour, both suicide deaths and highly lethal non-fatal attempts share similarities in demographics, clinical presentation, and neurobiological factors, suggesting a shared underlying vulnerability.
- The importance of diathesis alongside major psychiatric disorders is underscored by the fact that most individuals with such disorders never exhibit suicidal behaviours.
- Childhood adversity's epigenetic effects may further elevate suicide risk by amplifying mood disorder susceptibility through a diathesis mechanism.
- Genetic and epigenetic pathways to suicidal behaviour could connect genes with clinical and cognitive manifestations of biological intermediate phenotypes.
- This model offers a chance to merge neurobiological phenotypes with clinical and cognitive viewpoints.
- Brain regions involved in suicidal thoughts and behaviours are linked to emotion and impulse regulation.
- The ventral prefrontal cortex (VPFC) is associated with suicidal ideation
- The dorsal prefrontal cortex (DPFC) is linked to suicidal actions.
- The dorsal anterior cingulate cortex (dACC) and insula may facilitate the transition from suicidal thoughts to behaviours.
- Mental disorders with the highest suicide risk often show alterations in the VPFC, DPFC, dACC, and insula.
- Stressors such as life events and psychiatric disorders are important risk factors for suicide
- The diathesis concept explains why only a few individuals exposed to these risk factors with try to commit
- This can be shown through events like early-life adversity and epigenetic mechanisms
- Cross-sectional studies have shown that early-life adversity is one of te strongest risk factors of suicide, even after adjustment
- Experiences of repeated acts of abuse, especially physical and sexual abuse, increases the risk of suicidal behaviour throughout life
- Epigenetic mechanisms could explain the association between childhood experiences and reactivity to stressors later in life, mediated in part by the hypothalamic-pituitary-adreocortical axis.
- About 50% of the risk for suicide or suicide attempts is heritable
Neurological
Cells
- Post-mortem studies of people who have died by suicide show changes in several cell types, neurons and glial cells, which are the cells that hold nerve cells in place, and help them work in the way they should
- such as astrocytes, which perform metabolic, structural, homeostatic, and neuroprotective tasks. They provide structural support to neurons and help maintain the physical structure of the brain and spinal cord. Additionally, astrocytes regulate the extracellular environment surrounding neurons by maintaining the balance of ions and neurotransmitters. They play a crucial role in neurotransmitter uptake and recycling, helping to terminate synaptic transmission and prevent overstimulation of neurons. Astrocytes also provide metabolic support to neurons by supplying them with energy substrates and regulating blood flow in the brain
- And like oligodendrocytes, specialized cells in the central nervous system, that produce and uphold myelin which serves as an insulator, like the insulation on electrical wires, which accelerates and streamlines the transmission of nerve signals. This enhances the speed and efficiency of communication within the nervous system.
- Moreover, myelin contributes to the structural integrity of the axons it envelops, ensuring their stability and proper functioning over time. In essence, oligodendrocytes' generation and maintenance of myelin play a pivotal role in optimizing nerve signal conduction while supporting the structural integrity of the central nervous system.
- In the brainstem, suicide seems associated with more serotonin neurons, which regulate mood, emotion and behaviour and more tryptophan hydroxylase 2, an enzyme primarily found in the neurons of the brainstem, particularly in regions involved in the regulation of mood and emotion. Higher levels of TPH2 gene expression indicate increased production of mRNA molecules, leading to higher levels of TPH2 enzyme synthesis and possibly higher serotonin levels, compared with people who died suddenly as opposed to suicide and did not have a psychiatric illness.
- Both the serotonin neurons and tryptophan hydroxylase act as if the function of an insulator on electrical wires.
- Untreated depression who had died by suicide had fewer mature granule neurons in the hippocampus, specifically in the dentate gyrus which can lead to memory impairment, reduced neuroplasticity, disrupted emotional regulation, and cognitive decline. This was compared to people with depression given selective serotonin-reuptake inhibitors, which increase serotonin levels, before their death by suicide or people without a psychiatric disorder who died a sudden death that was not due to suicide.
- In parallel, in people with depression who died by suicide, the volume of the dentate gyrus is smaller, which affects memory, neuroplasticity, mood regulation, and cognitive function, and there is less angiogenesis, which can lead to an increased risk of cardiovascular events and compromised neurological function in people not treated than in those who were treated before death.
- The noradrenergic system utilizes norepinephrine as its primary neurotransmitter. It regulates arousal, attention, stress responses, mood, and autonomic functions throughout the body. There seems to be a deficiency of noradrenergic neurons in the locus coeruleus, a vital brainstem region, which can lead to reduced arousal, attention difficulties, development of mood disorder, cognitive impairments, and well as impaired stress responses of people who have died by suicide compared with individuals without psychiatric disorders who have died a sudden death.
- In mood disorders, three patterns of morphometric cellular changes are noted—cell loss including loss of glia (in the subgenual prefrontal cortex) which can disrupt neurotransmitter regulation, and contribute to mood and cognitive symptoms associated with psychiatric disorders. Another change is cell atrophy or lower neuronal density (dorsolateral prefrontal cortex and orbitofrontal cortex), which leads to structural and functional changes, impacting processes like decision-making and emotional regulation, which can lead to cognitive decline and mood disorders. The last cellular change is the increased number of serotonin cells (dorsal raphe nucleus), which has implications for mood regulations, emotional processing and various psychological functions.
Circuits
- Neuroimaging studies have established connections between brain circuitry, localized neurochemical changes, and components of the diathesis for suicidal behaviour such as mood regulation, reactive aggression, and decision-making.
- Functional MRI enables the observation of brain activity in specific regions, while molecular neuroimaging techniques allow for the quantification of neurotransmitter systems. By comparing individuals who have attempted suicide with control subjects with psychiatric disorders, researchers can directly investigate the underlying factors contributing to suicidal behaviour.
- Most molecular imaging studies have focused on the serotonin system. Two brain regions, one in the anterior cingulate, a region that regulates social functions and the medial prefrontal cortex, which integrates information from other brain regions and one in the lateral prefrontal cortex, which helps with cognitive control and executive function, as well as problem-solving and decision-making. These three were shown to have activity that was correlated with lethality (which is the degree of medical injury sustained as assessed with the Beck Medical Damage Scale) of suicidal behaviour in people with major depression.
- This relation, as measured by relative 18F-fluorodeoxyglucose (FDG) uptake on PET (refers to the measurement of glucose metabolism in specific regions of the body relative to a reference standard) was mediated by the degree of suicidal intent (positive correlation between the degree of intent and medical injury due to the attempt) and severity of impulsive trait (negative correlation between impulsivity and medical injury).
- The regional difference in brain activity between people who had made high-lethality suicide attempts and those who had made low-lethality suicide attempts was more pronounced in individuals given fenfluramine. This drug causes a robust release of serotonin. Prefrontal localized hypofunction(a specific part of the prefrontal cortex, which impacts cognitive and emotional functions) and impaired serotonergic responsivity(indicates reduced or altered functions of the brain’s serotonin system, which leads to disruption in mood regulation and emotional stability, and development of psychiatric disorders) in people who have attempted suicide were proportional to the lethality of suicide attempts.
- Later imaging studies showed that the uptake of 11C-methyltryptophan (an analogue of the essential amino acid tryptophan needed for the synthesis of serotonin) is low in the orbital medial prefrontal cortex(which would mean reduced serotonin activity, potentially affecting emotional processing and mood regulation) of people who have attempted suicide and in proportion to the degree of suicide intent.
- PET studies show a deficit of serotonin transporter binding in the serotonin neurons(which would suggest impaired serotonin reuptake, which affects serotonin neurotransmission, contributing to mood and psychiatric disorders) of people with depression who have attempted suicide compared with those of people with depression who did not attempt suicide or those of healthy individuals.
- This finding is similar to that of the deficit in serotonin-transporter expression and binding(which leads to impaired serotonin reuptake which affects serotonin neurotransmission, which can contribute to mood and psychiatric disorders) reported in post-mortem studies of people who have died by suicide.
- Conversely, investigators have noted higher brainstem 5-HT1A binding(increased activity of serotonin receptors in the brainstem, impacting mood regulation, emotional processing, and stress resilience) in people with depression who have attempted suicide, which was greatest in people who had higher intent and did more medical damage.
- These findings are consistent with lower transporter binding and higher 5-HT1A binding in the prefrontal cortex and brainstem(suggested altered serotonin activity, potentially impacting mood regulation, cognition, and emotional processing) of people who have died by suicide.Two studies showed no difference in dopamine-transporter binding(crucial for regulating dopamine levels and neurotransmission, influencing various brain functions, like movement, reward and motivation, and mood regulation) between people who attempted suicide and control individuals with depression, but more studies of other neurotransmitter systems are needed concerning suicidal behaviour.
- A further molecular imaging study investigated brain activity associated with the emotional pain of major depression that might lead to suicide. Greater emotional pain in individuals with depression was associated both with the risk of suicide and with changes in activity in several brain areas, including the dorsolateral prefrontal cortex(crucial for executive functions like working memory, decision-making and attentional control, regulating emotions, inhibiting impulsive responses, and understanding social cues) and the inferior frontal gyrus(involved in language processing, motor control, response inhibition, social cognition, empathy, and working memory manipulation ).Thus, despite the limited anatomical distribution of tracer targets and insufficient sensitivity to quantify the receptors in all brain regions(Limited anatomical distribution of tracer targets means the radiotracer used in imaging techniques binds to specific brain regions, not all. Insufficient sensitivity to quantify receptors in all brain regions suggests the imaging method may not accurately measure receptor concentration/activity in some areas. This limits the effectiveness of assessing certain brain regions.) where they are present, molecular imaging studies have begun to identify the neural circuitry of suicidal behaviour, and particularly, to implicate an abnormal serotonin system in more lethal suicidal behaviour.
- Imaging studies have explored further with the use of MRI the neural circuitry of individuals who show non-fatal suicidal behaviour Structural findings includes mainly right-sided deficits in volumes of grey matter in the orbitofrontal(decision-making, impulse control and emotional regulation), dorsolateral prefrontal(working memory, planning, and cognitive flexibility), insula(processing emotions, interoception, and social cognition), and superior temporal gyrus(auditory processing, language comprehension, and social perception) and basal ganglia(regulates movement, and is involved in motor control, procedural learning, and habit formation). The volumes of the thalamus(reflects its structural integrity and can influence sensory processing, and cognitive function) and right amygdala(reflects structural integrity and influences emotional processing and regulation) seem to be greater in suicide attempters. Findings of white-matter hyperintensities, particularly periventricular(cognitive decline, and increased stroke risk), increased bilateral volumes of inferior frontal white-matter tracts in the uncinate fasciculus and inferior orbitofrontal fasciculus(suggest structural changes in these brain regions that may have implications for cognitive and emotional processing) and lower anisotropy in the left orbitofrontal area and the left anterior limb of the internal capsule, indicate that there are structural connectivity impairments linked to suicidal behaviour.
Neurochemical
- Dopamine
- Recent scientific investigations have established a significant relationship between disruptions in dopaminergic function and the manifestation of suicidal behaviours. Specifically, alterations in dopamine levels and the expression of dopamine receptors, particularly within the dorsal striatum region of the brain which connects directly to decision-making, have been highlighted as potential factors influencing an individual's vulnerability to suicidal tendencies. These findings suggest that dysregulation of the dopaminergic system may contribute to the underlying mechanisms associated with suicidal behaviour, thereby warranting further exploration and understanding in this field of study
- Serotonin
- Serotonin, also known as 5-hydroxytryptamine (5-HT), is a monoamine synthesized by the rate-limiting enzyme tryptophan hydroxylase (TPH1 and TPH2) from tryptophan. It plays a crucial role in various nervous system functions such as mood regulation, anxiety, sleep, aggression, circadian rhythm, feeding, and social behaviour. Deficits in serotonin function are directly linked to depression and compulsivity, increasing the susceptibility to suicidal behaviour in both adolescents and adults.
- Clinical and genetic evidence implicates the serotonin transporter (SERT) in suicide risk. PET imaging studies have revealed reduced SERT abundance in the midbrain and elevated serotonin1A receptor levels in the raphe nuclei of individuals with depression who have attempted suicide. Postmortem brain tissue analysis has shown reduced SERT levels in the frontal cortex, hippocampus, and putamen, although findings vary depending on the brain region studied.
- Genetic variations, such as the polymorphism 5-HTTLPR in the serotonin transporter gene, are associated with a significantly higher risk of suicide, independent of age and sex. Overall, these findings highlight the critical role of serotonin and its transporter in the neurobiology of suicidal behaviour.
- Noradrenergic
- Noradrenaline, also known as norepinephrine (NE), is a catecholamine synthesized from tyrosine through enzymatic processes involving tyrosine hydroxylase (TH), aromatic L-amino acid decarboxylase (DDC), and dopamine β-hydroxylase (DβH). It serves as a neurotransmitter in both the central and peripheral nervous systems, regulating various cognitive functions, motivation, and impulsivity.
- Similar to serotonin, dysfunction in noradrenergic neurotransmission is strongly linked to depression and suicide, supporting the monoamine hypothesis. Studies have identified several polymorphisms in key components of the noradrenergic system, including DβH, norepinephrine transporter, and NE receptors, which are associated with depression, addiction, and suicide. These polymorphisms, whether they involve insertions, deletions, or amino acid changes, contribute to the susceptibility to these conditions.
Psychoneuroimmunolgical
- One of the most accepted ideas was the dysregulation of the immune system, which was sound in people with suicidal attempts
- This led to the hypothesis that cytokines are a risk marker for suicide in adolescence
- Data has shown that certain pro-inflammatory cytokines in adolescent suicide victims
- found elevated levels of cytokines in comparison to the control group
- The probable mechanisms for an increase in the levels of inflammatory cytokine levels might be due to the activation of toll-like receptors
- These receptors are known to play an essential role in regulating innate immune response and facilitating immune function
- mRNA and protein levels of TLR3 and TLR4 were consistently dysregulated
- these receptors have garnered attention for their possible role in the inflammatory response, which has been implicated in psychiatric disorders including depression and suicidal behaviour. We discuss how alterations in TLR3 and TLR4 expression or function may contribute to chronic inflammation, impacting neurotransmitter function, neuroplasticity, and mood regulation
- Inflammatory cytokines are interlinked with suicidal behaviours
- The cytokines IFN-γ (Interferon-gamma), IL-6 (Interleukin-6), IL-1β (Interleukin-1 beta), and TNF-α (Tumor Necrosis Factor-alpha) are known to play critical roles in the immune response and inflammation. In the context of suicidal behavior in adolescents, alterations in the levels or activity of these cytokines have been observed.
- 1. IFN-γ is primarily produced by activated T cells and natural killer cells in response to pathogens. It plays a key role in modulating immune responses, including promoting inflammation and activating macrophages. In suicidal adolescents, elevated levels of IFN-γ have been reported, suggesting increased immune activation and inflammatory processes.
- 2. IL-6 is a multifunctional cytokine produced by various cell types, including immune cells and endothelial cells. It has both pro-inflammatory and anti-inflammatory effects and is involved in regulating immune responses, acute-phase reactions, and hematopoiesis. Elevated levels of IL-6 have been associated with psychiatric disorders, including depression, and may contribute to neuroinflammation and synaptic dysfunction observed in suicidal individuals.
- 3. IL-1β is produced mainly by activated macrophages and monocytes in response to infection or injury. It plays a central role in initiating and amplifying inflammatory responses and is implicated in the pathophysiology of various inflammatory and autoimmune diseases. Dysregulation of IL-1β has been linked to mood disorders and suicidal behaviour, with increased levels observed in some studies involving adolescents.
- 4. TNF-α is produced primarily by activated macrophages and T cells and plays a crucial role in inflammation, apoptosis, and immune regulation. Elevated levels of TNF-α have been reported in individuals with depression and other psychiatric disorders, suggesting its involvement in the pathophysiology of mood disorders and suicidal behaviour.
- Activation of the kynurenine pathway
- In the context of suicidal behaviour, several studies have reported abnormalities in the kynurenine pathway, including elevated levels of kynurenine and its metabolites, such as QUIN, in the blood, cerebrospinal fluid, and brain tissue of individuals who have died by suicide or who have suicidal ideation. These findings suggest that the activation of the kynurenine pathway may contribute to the neurobiological mechanisms underlying suicidal behaviour.
- Dysregulation of the HPA axis
- During periods of stress, the hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to produce adrenocorticotropic hormone (ACTH). ACTH then stimulates the adrenal glands to release cortisol, the primary stress hormone. Cortisol exerts widespread effects on the body, including regulating metabolism, immune function, and stress response.
- Dysregulation of the HPA axis can manifest in several ways, including hyperactivity or blunted responsiveness of the axis. In individuals with suicidal behaviour or mood disorders, abnormalities in HPA axis function have been observed, including:
- 1. Hyperactivity of the HPA axis: Some individuals with suicidal behaviour exhibit hyperactivity of the HPA axis, characterized by elevated levels of cortisol or increased responsiveness to stressors. Chronic exposure to stressors may lead to sustained elevations in cortisol levels, which can have detrimental effects on the brain, including impairments in neuroplasticity, hippocampal atrophy, and dysregulation of neurotransmitter systems implicated in mood regulation.
- 2. Blunted HPA axis responsiveness: Conversely, some individuals may exhibit blunted responsiveness of the HPA axis, characterized by reduced cortisol levels or diminished cortisol responses to stress. This blunted responsiveness may reflect adaptations to chronic stress exposure or may be indicative of a state of allostatic load, where the body's ability to adapt to stressors is compromised. Blunted cortisol responses have been associated with increased risk of suicidal behavior and may reflect alterations in feedback mechanisms within the HPA axis.
- Alterations in monoamine metabolism
- Alterations in monoamine metabolism, particularly involving neurotransmitters such as serotonin, dopamine and norepinephrine, have been implicated in the pathophysiology of suicide. These play crucial roles in regulating mood, motivation, impulse control, and dysregulation of their metabolism has been associated with various psychiatric disorders, including depression and schizophrenia.
- alterations in monoamine metabolism are thought to contribute to the neurobiological mechanisms underlying suicidal behaviour, including alterations in mood regulation, impulse control, and stress response. Pharmacological interventions targeting monoamine neurotransmitter systems, such as selective serotonin reuptake inhibitors (SSRIs) or monoamine oxidase inhibitors (MAOIs), are commonly used in the treatment of depression and other mood disorders associated with suicide risk. However, the precise mechanisms by which alterations in monoamine metabolism contribute to suicidal behaviour remain to be fully elucidated, and further research is needed to identify novel therapeutic targets for suicide prevention and intervention.
Biological Factors
- Suicidal Crisis
- A suicidal crisis refers to a state of heightened emotional distress and cognitive instability which leads to suicidal thoughts, impulses, or behavious
- During a suicidal crisis, various neurobiological processes may be involved, including alterations in neurotransmitter levels(such as serotonin, dopamine, and norepinephrine)
- changes in brain circuitry related to mood regulation and impulse control and dysregulation of stress response (such as the hypothalamic-pituitary-adrenal axis which is the axis that plays a crucial role in the body's response to stress, but dysregulation contribute to various physical and mental health problems)
- These biological factors can contribute to the intense emotional pain, hopelessness, and impaired decision making a common experience during a suicidal crisis
- additionally, genetic predispositions, and environmental factors may interact with these biological mechanisms
- External/Internal Destabilizing Factors
- External and Internal Destabilizing factors refer to circumstances or conditions that can contribute to an individual vulnerability to suicidal thoughts, impulses or behaviours
- External Destabilizing Factors
- environmental or situational factors outside of the individual that may increase suicide risk
- examples include: relationship problems or conflicts, financial difficulties of job loss, traumatic life events such as loss of a loved one or exposure to violence, legal or disciplinary issues, social isolation or lack of social support
- Internal Destabilizing Factors
- are factors within the individual that may increase suicide risk
- examples include relationship problems or conflicts, financial difficulties or job loss, traumatic life events such as loss of a loved one or exposure to violence, legal or disciplinary issues, social isolation or lack of social support
- Salutogenesis vs. Pathogenesis imbalance
- Salutogenesis
- focuses on identifying and promoting factors that contribute to health , well-being, and resilience. It emphasizes understanding the factors that support individuals in maintaining or enhancing their health, rather than focusing or risk factors or disease pathology.
- In the context of suicide prevention, a salutogenic approach would involve identifying and bolstering protective factors such as social support, coping skills, sense of purpose and resilience, to promote mental health and suicide risk.
- Pathogenesis,
- focuses on identifying and addressing factors that contribute to the development and progression of disease or negative outcomes.
- it emphasizes understanding the underlying causes and mechanisms of illness or dysfunction
- in the context of suicide prevention, a pathogenic approach would involve identifying and addressing risk factors , such as mental health disorders, substance abuse, trauma, and environmental stressors that contribute to suicidal thoughts or behaviors.
- Salutogenesis
- Structual and functional neural circuitry dysfunction
- Structural dysfunction
- involves alterations in the physical organization and connectivity in neural circuits.
- It may include changes in the density, morphology, or integrity of neurons, as well as abnormalities in the formation or maintenance of syaptic connects between neurons. structural dysfunction can result from various factors such as genetic mutations, developmental abnormalities, traumatic brain injury, neurodegenerative diseases, or exposure to toxins.
- Functional Dysfunction
- refers to abnormalities in neurotransmitter in the pattern of activity or communication within neural circuits
- It encompasses alterations in neurotransmitter release, synaptic transmission, neural oscillations, and network connectivity. Functional dysfunction can manifest as aberrant neural activation patterns, disrupted information processing, or dysregulated neurochemical signaling. It may underlie cognitive, emotional, or behavioural symptoms associated with psychiatric disorders, neurological conditions, or other brain-related disorders.
- refers to abnormalities in neurotransmitter in the pattern of activity or communication within neural circuits
- Structural dysfunction
- Dysregulation of neurotrophic factories, inflammation, HPA axis
- Neurotrophic Factors: Neurotrophic factors are proteins that support the growth, survival, and function of neurons in the brain. Dysregulation of neurotrophic factors, such as brain-derived neurotrophic factor (BDNF), can disrupt neuroplasticity, synaptic connectivity, and neuronal survival, contributing to mood disorders like depression and anxiety. Low levels of BDNF, for example, have been associated with decreased resilience to stress and increased susceptibility to psychiatric disorders.
- Inflammation
- Inflammation in the brain, known as neuroinflammation, involves the activation of immune cells and release of pro-inflammatory molecules in response to injury, infection, or stress. Chronic neuroinflammation has been implicated in the pathophysiology of various psychiatric and neurological disorders, including depression, schizophrenia, and Alzheimer's disease. Elevated levels of inflammatory markers in the blood or cerebrospinal fluid have been observed in individuals with mood disorders, suggesting a link between inflammation and mental health.
- HPA Axis:
- The HPA axis is a key neuroendocrine system involved in the body's response to stress. Dysregulation of the HPA axis, characterized by abnormal cortisol levels or impaired feedback mechanisms, can lead to chronic stress, hyperarousal, and altered mood regulation. Chronic activation of the HPA axis has been associated with increased risk of depression, anxiety disorders, and other stress-related conditions. Additionally, dysfunction of the HPA axis can contribute to alterations in neurotransmitter systems, neuroplasticity, and inflammation, further impacting mental health.
- Congenital and Acquired epigenetic modifications
- Congenital Epigenetic Modifications: These are alterations in gene expression patterns that occur early in development and are inherited or present from birth. They can result from environmental factors experienced by previous generations, such as prenatal stress, maternal nutrition, or exposure to toxins. Congenital epigenetic modifications can affect the development and function of brain circuits involved in mood regulation, stress response, and impulse control, increasing susceptibility to mental health disorders and suicidal behavior later in life.
- Acquired Epigenetic Modifications: These are changes in gene expression patterns that occur throughout life in response to environmental influences or experiences. Acquired epigenetic modifications can be triggered by factors such as stress, trauma, substance abuse, or chronic illness. They can alter the activity of genes involved in stress regulation, neurotransmitter signaling, and synaptic plasticity, contributing to the development or exacerbation of mental health disorders and suicidal tendencies. Acquired epigenetic modifications may also interact with genetic predispositions to further increase suicide risk.
- Acute/Chronic stressful stimuli
- Acute Stressful Stimuli: These are sudden, short-lived events or situations that pose an immediate threat or challenge to an individual's well-being. Examples include traumatic events, such as accidents, natural disasters, or interpersonal violence, as well as acute life crises, such as sudden loss of a loved one or financial crisis. Acute stressors can trigger intense emotional distress, overwhelm coping mechanisms, and lead to a temporary increase in suicide risk, especially in individuals already predisposed to mental health issues.
- Chronic Stressful Stimuli
- These are persistent, ongoing conditions or circumstances that exert prolonged pressure or strain on an individual's physical, emotional, or psychological resources. Examples include chronic illness, long-term caregiving responsibilities, abusive relationships, or socioeconomic hardship. Chronic stressors can disrupt neurobiological systems involved in stress response, such as the hypothalamic-pituitary-adrenal (HPA) axis and the autonomic nervous system, leading to dysregulation of mood, cognition, and behavior. Over time, chronic stress can contribute to the development or exacerbation of mental health disorders, including depression, anxiety, and post-traumatic stress disorder (PTSD), which are associated with increased suicide risk.
- Genetic Background
- Genetic Predisposition: Genetic background contributes to an individual's inherent susceptibility to mental health disorders, personality traits, and physiological processes that influence suicide risk. Certain genetic variations or mutations may increase the likelihood of developing psychiatric conditions such as depression, bipolar disorder, schizophrenia, or substance abuse disorders, all of which are associated with heightened suicide risk.
- Heritability of Suicide Risk: Studies have shown that suicide risk has a heritable component, with genetic factors estimated to account for approximately 30-50% of the variability in susceptibility to suicidal behavior. This suggests that individuals with a family history of suicide or mental illness may be at increased genetic risk for suicidal tendencies.
- Gene-Environment Interactions: Genetic predispositions to suicide interact with environmental factors, such as early-life adversity, trauma, social stressors, or access to lethal means, to influence the likelihood of suicidal behavior. Gene-environment interactions can modulate neurobiological pathways involved in stress response, emotion regulation, impulsivity, and decision-making, contributing to the development or exacerbation of suicidal tendencies.
- Polygenic Risk Scores: Advances in genetic research have led to the identification of multiple genetic variants associated with suicide risk. Polygenic risk scores, which aggregate information from numerous genetic markers, can help predict an individual's genetic predisposition to suicidal behavior, although their utility in clinical practice is still being evaluated.
- Genetics
- Certain genetic factors, combined with environmental influences, can contribute to suicidal behaviour, particularly in adolescents.
- Let's start with the serotonin transporter, abbreviated as 5-HTT. Think of 5-HTT as a bus system in our brains that helps move around a chemical called serotonin, which plays a big role in regulating mood and happiness.
- Now, within our genetic makeup, there's a specific area called the serotonin transporter gene, and within that, there's a region called 5-HTTLPR. This area is like a switch that can be influenced by things like stress. When stress hits, it can affect how this switch behaves.
- Within this switch, there are two variations, or alleles: the s-allele and the l-allele. These alleles affect how much serotonin transporter gets produced. The s-allele tends to produce less of it compared to the l-allele.
- Studies have shown that individuals who have attempted suicide tend to have a higher prevalence of the s-allele. So, it's like having more of those switches that produce less serotonin transporter, potentially leading to lower levels of serotonin moving around in the brain, which can affect mood.
- But genetic factors are just one piece of the puzzle. Other factors come into play, such as the levels of a protein called BDNF, which supports brain health, and the regulation of a hormone called CRH, which is involved in stress responses.
- Additionally, childhood experiences can significantly impact mental health outcomes. Childhood abuse, for example, can further complicate matters. It's like adding more layers to the puzzle, making it even more intricate and challenging to navigate.
- So, when you combine all these factors—genetic predispositions, chemical imbalances, and environmental stressors—it creates a complex landscape where suicidal behaviour can emerge, especially in vulnerable populations like adolescents.
- Epigenetic markers
- Our DNA, which contains the instructions for building and operating our bodies, can undergo a complex process called epigenetics. Think of epigenetics like a layer of instructions on top of our DNA, influencing how genes are turned on or off without changing the actual genetic code.
- One important aspect of epigenetics is methylation, where chemical groups called methyl groups are added to our DNA or the proteins surrounding it, known as chromatin. These methyl groups act like switches, controlling whether certain genes are activated or not, thus affecting how our bodies function.
- Now, here's where it gets interesting: experiences we go through, particularly during childhood, can alter these methylation patterns. For example, exposure to stress or trauma during childhood can lead to changes in the methylation of genes related to suicidal behaviour in adolescents.
- Researchers have found that specific genes, such as those involved in the regulation of stress hormones like corticotropin-releasing hormone (CRH), can have altered methylation patterns in individuals who have attempted suicide. This suggests that changes in gene methylation could be used as biomarkers to identify individuals at risk of suicidal behaviour.
- Furthermore, studies have shown that childhood abuse or trauma can lead to changes in methylation patterns in genes associated with brain function and mental health. These changes can impact the functioning of genes related to the hypothalamic-pituitary-adrenal (HPA) axis, which regulates the body's response to stress.
- For instance, researchers have identified specific methylation patterns in genes like CRH and NR3C1 (involved in stress response) in individuals who have experienced childhood abuse and are at risk of suicide. These changes in gene methylation can affect how these genes function, potentially increasing vulnerability to suicidal ideation.
- In summary, epigenetic changes, particularly in gene methylation, play a significant role in influencing our susceptibility to mental health issues, including suicidal behaviour. Understanding these mechanisms may lead to the development of strategies for early identification and intervention to support individuals at risk.
-
Neuroendocrine Dysregulation
-
Beyond the HPA axis, dysfunctions in other neuroendocrine systems, such as the hypothalamic-pituitary-thyroid (HPT) axis and the hypothalamic-pituitary-gonadal (HPG) axis, have been implicated in suicidal behavior. Abnormalities in hormone levels, including thyroid hormones and sex hormones, may contribute to altered mood states and vulnerability to suicide.
-
-
Neuroplasticity
-
Changes in neuroplasticity, the brain's ability to reorganize and adapt, have been observed in individuals at risk for suicide. Alterations in synaptic connectivity, neurogenesis, and the expression of neurotrophic factors may impact mood regulation and resilience to stress, influencing suicide risk.
-
- Mitochondrial Dysfunction
- Emerging research suggests a potential link between mitochondrial dysfunction and suicidal behaviour. Mitochondria are crucial for energy production and cellular function, and disruptions in mitochondrial integrity and function may contribute to neuronal dysfunction and oxidative stress, both of which are implicated in psychiatric disorders and suicide risk.
- Immune System Dysregulation
- In addition to chronic inflammation, alterations in immune function, including abnormalities in cytokine levels and immune cell activity, have been associated with suicidal behaviour. Immune dysregulation may contribute to neuroinflammation and affect neurotransmitter systems involved in mood regulation.
- Oxidative Stress
- Increased oxidative stress, resulting from an imbalance between reactive oxygen species (ROS) production and antioxidant defences, has been implicated in the pathophysiology of psychiatric disorders, including depression and suicidality. Oxidative damage to neuronal cells may contribute to neurodegeneration and exacerbate psychiatric symptoms.
- Gut Microbiota
- The gut microbiota-gut-brain axis represents bidirectional communication between the gut microbiota and the central nervous system. Alterations in the composition and diversity of gut microbiota, known as dysbiosis, have been linked to psychiatric disorders and may influence mood, behaviour, and susceptibility to suicidal behaviour through neuroimmune and neuroendocrine pathways.
- Sleep Disturbances
- Disruptions in sleep architecture and circadian rhythms are common in individuals with psychiatric disorders and may contribute to suicidal behaviour. Sleep disturbances, including insomnia and hypersomnia, can exacerbate mood symptoms, impair cognitive function, and increase impulsivity, all of which are risk factors for suicide.
- Endocrine System
- Thyroid dysfunction and abnormalities in other endocrine systems have been linked to depression and suicidal behaviour. Thyroid hormones play a crucial role in regulating mood and metabolism, and alterations in thyroid function may contribute to depressive symptoms and suicide risk.
- Neurotransmitter Receptor Abnormalities
- Changes in the density, distribution, and function of neurotransmitter receptors, such as serotonin receptors (5-HT1A, 5-HT2A), glutamate receptors (NMDA, AMPA),which are essential for various brain functions including learning, memory, and synaptic plasticity, and gamma-aminobutyric acid (GABA) receptors, essential for regulating various physiological processes, including anxiety and stress, sleep, motor control, and cognition, have been observed in individuals with suicidal behaviour. These alterations may disrupt neurotransmission and contribute to mood dysregulation and impulsivity.
- Opioid System Dysregulation
- Alterations in the endogenous opioid system, including changes in opioid receptor expression and opioid peptide levels, have been reported in individuals with suicidal behavior. Dysfunctions in the opioid system may influence pain perception, emotional processing, and stress response, contributing to suicide risk.
- Neurohormonal Alterations
- Dysregulation of neurohormonal systems, such as the vasopressin system and the oxytocin system, has been implicated in suicidal behavior. Abnormalities in the secretion and function of neuropeptides, such as vasopressin and oxytocin, may affect social bonding, stress response, and emotional regulation.
- Neurotensin System Dysregulation
- Dysfunctions in the neurotensin system, a neuropeptide system involved in pain modulation, stress response, and emotional behavior, have been associated with suicidal behavior. Altered levels of neurotensin and abnormalities in neurotensin receptor signaling may contribute to mood disorders and impulsivity.
Psychological
Personality Traits:
1. Hopelessness:
- Feeling hopeless about the future is a significant predictor of suicidal ideation and behavior.
- Individuals who perceive no way out of their current situation may see suicide as the only option to escape their pain.
2. Purposelessness:
- Lack of a sense of purpose or meaning in life can contribute to feelings of despair and hopelessness, increasing vulnerability to suicidal thoughts.
- Adolescents who lack direction or goals may struggle to cope with challenges, increasing their risk of suicidal behavior.
3. Trapped:
- Feeling trapped in adverse circumstances or emotional distress can intensify suicidal ideation.
- Perceiving no escape from overwhelming problems can lead individuals to consider suicide as a way to end their suffering.
4. Impulsivity:
- Impulsivity is strongly associated with suicidal behavior, as individuals may act on suicidal thoughts without fully considering the consequences.
- Adolescents with high impulsivity may engage in reckless behaviors or suicide attempts without adequate planning or forethought.
5. Aggression:
- Aggressive tendencies, including hostility and anger, are risk factors for suicidal behavior, especially when combined with other risk factors like substance abuse or trauma.
- Adolescents with aggressive traits may have difficulty regulating their emotions, leading to impulsive and harmful actions.
6. Perfectionism:
- High levels of perfectionism, characterized by unrealistic standards and fear of failure, increase the risk of suicidal ideation and attempts.
- Adolescents who feel they cannot meet their own or others' expectations may become overwhelmed and hopeless, seeing suicide as a solution to escape perceived failure.
7. Self-Efficacy:
- Self-efficacy, or belief in one's ability to accomplish tasks and overcome challenges, can act as a protective factor against suicide.
- Adolescents with high self-efficacy may be better equipped to cope with stress and setbacks, reducing their risk of suicidal behavior.
8. Locus of Control:
- Locus of control refers to the extent to which individuals believe they have control over their lives.
- Adolescents with an external locus of control, believing that external factors dictate their fate, may feel powerless to change their circumstances, increasing suicide risk.
9. Neuroticism:
- High levels of neuroticism, characterized by emotional instability and negative affect, are associated with increased risk of suicidal behavior.
- Adolescents prone to neuroticism may experience heightened distress and difficulty coping with life's challenges, making them more susceptible to suicidal thoughts.
Cognitive Factors:
1. Rigidity:
- Cognitive rigidity, characterized by inflexible thinking and difficulty adapting to new situations, is associated with increased suicide risk.
- Adolescents with cognitive rigidity may struggle to problem-solve or seek alternative solutions to distressing situations, increasing feelings of hopelessness.
2. Thought Suppression:
- Attempting to suppress unwanted thoughts or emotions can backfire and intensify them, contributing to suicidal ideation.
- Adolescents who engage in thought suppression may find it difficult to cope with distressing thoughts, increasing their risk of suicidal behavior.
3. Fearlessness:
- Fearlessness of death or pain sensitivity may reduce barriers to suicidal behavior.
- Adolescents with high fearlessness may be more likely to engage in risky or self-destructive behaviors, including suicide attempts.
4. Pain Sensitivity:
- Heightened pain sensitivity or tolerance may influence an individual's willingness to engage in self-harm or suicidal behavior.
- Adolescents who perceive pain differently or have a high pain threshold may be more likely to engage in behaviors that pose physical harm, including suicide attempts.
5. Agitation:
- Agitation and restlessness can exacerbate feelings of distress and impulsivity, increasing suicide risk.
- Adolescents experiencing agitation may struggle to cope with emotional turmoil, leading to impulsive and potentially harmful actions.
6. Implicit Associations:
- Implicit associations between self and death or suicide-related concepts can influence suicidal behavior.
- Adolescents with strong implicit associations between themselves and suicide may be at heightened risk for suicidal ideation and attempts.
Mental
- Mood disorders are most commonly associated with a diagnosis of suicidal ideation in adults, as well as adolescents
- Major Depressive Disorder and Dysthymia
- Major depression which is often episodic, recurrent, or even chronic is diagnosed upon the occurrence of a major depressive episode. A major depressive episode includes at least five of a list of nine criteria symptoms persisting for a minimum of 2 weeks including: depressed or irritable mood, diminished interest in usual activities and pleasures, changes in eating and sleeping, and suicidal thoughts.
- Dysthmic disorder is when an individual is sad and depressered more days tha not for at least two years, but doesnt have the symptoms for a major depressive disorders
- More than half of those with depressive disorders have thoughts of suicide. The severity of the ideation increases with the intensity of the disorder. A study of over 35,000 insured people receiving treatment showed greater rates of suicide by those receiving more intensive treatments. The highest suicide rate was among those receiving inpatient treatments, which is a form of care for high-risk suicide pateints, which invloves admitting them to a psychiatric facilities. The least was with outpatient treatment with medication, which involves This type of care provides ongoing support, therapy, and monitoring for individuals while allowing them to continue living in their communities and maintaining their daily routines. NO suicide was observed in those being treated on an outpatient basis.
- Other depressive symptoms predictive of suicidality are hopelessness (Beck et al., 1975; Beck, 1986) as well as feelings of guilt, loss of interest in usual activities, and low self-esteem
- Bipolar Disorder
- 25 to 50% of the U.S population with Bipolar Disorder will attempt suicide at least once
- Bipolar Disorder has significant genetic heritability and includes depressive and manic disorders
- Depressive epusodies as descriped before, can include long-lasting sad, apathetic or irritable mood, altered thinking, activity and bodily functions.
- Severity of the disorder is also associated with increased risk for suicide, and those with more severe cases of bipolar disorder will have more frequent hospitilizations
- Suicide risk is higher in people with bipolar type II disorder, which includes hypomanic episodes but not mania.
- According to one study, of 100 consecutive suicides, 46% had bipolar II, 1% had bipolar I, and 53% had significant depressive illness that was not bipolar disorder. Bipolar II patients may be especially vulnerable because they experience more mixed moods, which can include extreme agitation along with concurrent manic and depressed symptoms.
- People with bipolar disorder have a markedly higher incidence of alcohol and/or drug use disorders, which is partially explained by their desire to "self-medicate." The rates of suicide that are linked to the co-occurrence of these two disorders are higher than the rates for each disorder alone.
- Anxiety Disorder
- A recent study using the National Comorbidity Survey data found that all anxiety disorders including PTSD, the population attributable risk for serious suicide attempts is 60% for femals and 43% for males
- Panic Disorder
- Studies by Weissman et al. (1989) have revealed a significant correlation between panic disorder and suicide attempts, with individuals suffering from panic disorder exhibiting nearly a 20-fold increased risk compared to those without any psychiatric disorder. Follow-up investigations, such as those conducted by Schmidt et al. (2000), have shown that panic disorder contributes to approximately 20% of suicide deaths, establishing it as a substantial risk factor. Notably, comorbidity with other mental illnesses exacerbates this risk, particularly when accompanied by depression and agoraphobia.
- Post-Traumatics Stress Disorder
- Research indicates that PTSD exhibits one of the strongest associations with suicidality among anxiety disorders. Studies by Kessler et al. (1999) have demonstrated that individuals with PTSD have a significantly elevated risk of making impulsive suicide attempts and formulating suicide plans compared to those with other anxiety disorders. Furthermore, the physiological and neurobiological alterations observed in PTSD, including dysregulation of stress hormones and abnormalities in brain regions associated with emotion and memory, contribute to the development of suicidal behaviors
- Scizophrenic Disorder
- Individuals with schizophrenic disorders face a profound risk of suicide, with rates approximately 30 to 40 times higher than the general population, as indicated by studies cited by Caldwell and Gottesman (1992) and Harris and Barraclough (1998). This elevated risk persists throughout the course of the disorder, with peaks early in the illness and following discharge from psychiatric care. Positive symptoms of schizophrenia, such as command hallucinations, and co-occurring depressive symptoms significantly contribute to increased suicide rates among this population.
- Personality Disorders, Particularly Borderline Personality Disorder (BPD),
- BPD represents a significant risk factor for suicide, with approximately 10% of individuals with this disorder eventually dying by suicide, as indicated by Frances et al. (1986) and Stone et al. (1987). The propensity for impulsive and self-destructive behaviors, combined with high rates of comorbidity with mood and substance use disorders, underscores the severity of suicidality in this population. Childhood trauma, often prevalent among individuals with BPD, further amplifies suicide risk, emphasizing the importance of trauma-informed care in suicide prevention efforts.
- Alcohol Use Disorders
- Alcohol use disorders are strongly associated with increased suicide risk, with alcohol-related suicides being more prevalent in certain regions, as noted by Hlady and Middaugh (1988). The disinhibiting effects of alcohol, coupled with its association with mood disturbances and impulsivity, contribute to a higher likelihood of engaging in suicidal behaviors among individuals with alcohol use disorders. Additionally, the presence of alcohol-related suicides across various methods underscores the multifaceted nature of this relationship and the need for comprehensive prevention strategies targeting both substance use and suicidality.
- Prevalence of Mental Disorders in Youth
- The provided data indicates that a significant portion of children and adolescents experience mental disorders, with about 20% exhibiting at least mild functional impairment. Mood disorders, including major depressive episodes, are identified in 6.2% of this population. Moreover, longitudinal studies from New Zealand reveal a notable increase in the prevalence of DSM-III disorders from adolescence to young adulthood, indicating the evolving nature of mental health challenges during this developmental period.
- Suicide Risk Factors in Adolescents
- Depression emerges as a significant risk factor for suicide among adolescents, supported by various studies cited in the text. While depression is highlighted as the primary correlate of suicide, conduct disorder also plays a notable role in suicide attempts among adolescents. Additionally, personality disorders are implicated in a substantial proportion of youth suicides, suggesting the importance of addressing complex psychiatric comorbidities in suicide prevention efforts.
- Nature of Mental Disorders in Youth
- The symptom presentation of mental disorders in children and adolescents may differ from that observed in adults. Youth are more likely to display irritability, acting out behaviours, and anger, rather than overtly sad or depressed affect. Furthermore, bipolar disorder in youth often presents with symptoms commonly associated with conduct disorder or attention deficit disorder, complicating diagnostic processes and necessitating tailored treatment approaches.
- Alcohol and Substance Abuse in Adolescents
- Substance abuse, particularly alcohol use, is identified as a significant risk factor for suicide among adolescents. The text underscores the strong link between alcohol use and suicide, particularly among youth who use firearms to complete suicide. Substance abuse, including alcohol and illicit drugs, has been implicated in the rise in adolescent suicide rates observed in the United States, highlighting the need for targeted prevention and intervention strategies.
- Comorbidity of Psychiatric Disorders
- Co-occurrence of mental disorders with substance use disorders or somatic disorders significantly amplifies the risk of suicide among adolescents. The text suggests that methodological challenges in psychiatry, such as focusing solely on a single "primary" diagnosis, may obscure the understanding of the heightened suicide risk associated with comorbidity. Addressing comorbid psychiatric conditions and substance abuse is crucial for comprehensive suicide prevention efforts among youth.
- Major Depressive Disorder and Dysthymia
Social
- Social Transmission
- When a close family member attempts or commits, it can increase tendencies, especially when it comes from maternal aspects
- Parental suicide has a more detrimental effect on children
- Social Isolation
- Indicative of suicidal behaviours because of the lack of support and vulnerability of the individual to negative factors such as stress
- Social Media and Networking
- Shown a negative impact on adolescents and has ked to self-harming and suicidal ideation
- Critical when analyzing suicidal behaviour
- Social Isolation and Social Distancing
- COVID-19 showed an increase in risks for mental health issues, such as fear, anxiety, and increased suicidal risk.
- Negative Life Event
- Childhood Adversities
- Early-life stress can lead to suicidal behaviour
- While the type of adversity affects the individual
- The extent may vary according to the kind of stress experience
- Traumatic Life Events During Adulthood
- Traumatic experiences can affect any individual at any age, and could potentially lead to suicidal ideations
- Physical Illness
- Associated with suicidal behaviours
- Childhood Adversities
- Peer Relationships
- Adolescents are highly influenced by their peer groups. Issues such as social rejection, bullying, peer pressure, and social isolation can significantly impact their mental health and increase the risk of suicidal behaviour.
- Family Environment
- Family dynamics, including parental relationships, family conflict, abuse (physical, emotional, or sexual), neglect, and dysfunctional family structures, can contribute to feelings of hopelessness and despair in adolescents.
- Academic Pressure
- High academic expectations, academic failure, and performance-related stress can exacerbate feelings of inadequacy and worthlessness in adolescents, leading to suicidal thoughts and behaviors.
- Social Media and Cyberbullying
- The rise of social media has introduced new challenges for adolescents, including cyberbullying, online harassment, and comparison with others, which can negatively impact self-esteem and mental well-being.
- Substance Abuse
- Substance abuse, including alcohol and drug use, is strongly linked to suicidal behavior among adolescents. Substance abuse can impair judgment, exacerbate existing mental health issues, and increase impulsivity, all of which elevate the risk of suicide.
- Cultural and Societal Norms
- Cultural and societal attitudes towards mental health, suicide, and help-seeking behaviour can influence whether adolescents feel comfortable seeking support. The stigma surrounding mental illness may prevent adolescents from seeking help, exacerbating their distress.
- Traumatic Events
- Exposure to trauma, such as violence, the loss of a loved one, or witnessing traumatic events, can significantly impact adolescent mental health and increase the risk of suicidal behaviour.
- Sexual Orientation and Gender Identity
- LGBTQ+ adolescents face unique social challenges, including discrimination, rejection from family or peers, and lack of support, which can contribute to feelings of isolation and distress, increasing their vulnerability to suicide.
- Access to Lethal Means
- Easy access to lethal means, such as firearms or prescription medications, increases the likelihood of impulsive suicide attempts among adolescents.
- Racial and Ethnic Discrimination
- Experiences of discrimination contribute to higher rates of depression, anxiety, and suicidal behavior among these adolescents. Cultural factors and barriers to accessing culturally competent mental health care exacerbate these challenges.
Acute Grief
- After death, individuals may experience intense and distressing emotions, regardless of the cause
- bereaved individuals often experience feelings of numbness, shock and denial.
- For some, this provides a brief response to the pain and as an initial response, allowing time and energy to deal with practical implications.
- The full impact of the death will not be comprehended emotionally and cognitively, until integrated grief
Integrated Grief
- Acute Grief typically evolves into integrated grief within a few months, but this process may be prolonged for those bereaved by suicide.
- However, as described later, this period may be substantially extended for those who have lost a loved one to suicide.
- Healing from the loss involves recognizing the grief experienced, leading to the emergence of new capacities, wisdom, and strengths in the aftermath.
- However, a minority of individuals may struggle to recognize their grief and may develop complicated grief reactions characterized by prolonged distress and difficulty functioning.
Complicated Grief
- Complicated grief is a bereavement reaction characterized by prolonged acute grief that causes distress and interferes with functioning.
- Individuals experience persistent longing and yearning for the deceased, difficulty in re-establishing a meaningful life without them, and a sense that the pain of the loss remains fresh and unhealed
- The pain of the loss stays fresh and healing does not occur.
- The bereaved person feels stuck; time moves forward but the intense grief remains
- Symptoms include recurrent intense grief, preoccupation with the deceased, avoidance of reminders of the loss, intrusive images of the death, and difficulty experiencing positive memories.
- Life may feel empty, and the yearning may lead to suicidal thoughts and behaviours, or the belief that death is the only relief from the intense pain of the loss(suicidal ideation).
- .Alternatively, the pain from the loss may be so intense that their death may feel like the only possible outlet or option
Complicated Grief in Survivors of Suicide
-
Data indicates a high incidence of Complicated Grief (CG) among survivors of suicide loss, with these individuals at elevated risk of developing CG.
-
Those who develop CG are nearly 10 times more likely to report suicidal ideation one month after the death of their loved ones, even after controlling for depression.
-
In comparison to other bereaved individuals, suicide-bereaved participants report twice the rate of recurrent and current depression, higher rates of suicidal ideation before the death, and are at least as likely to report suicidal ideation afterward.
Data
As of now, my data is as follows.

I investigated receiving data, through dataming from social media platforms, specifically Reddit and Quora. Through that, these are my findings. The responses that I found were for the question, "If someone tells others that they are thinking or planning suicide, what are people's responses?"
1. Relating to Person: they are thinking or wanting to commit suicide.
2. Alleviation: making them feel better as a person and attempting to alleviate negative emotions
3. Engaging: somehow extending the conversation so they can better understand the concept and give them
tailored advice
4. Help Advising: telling them to go seek help in a professional medical setting
5. Suggestion: giving them essential home remedies to solve their ideations
6. Science: using science to help them figure out what is biologically happening and using that to help solve
their issue
7. Spirituality: using religion or spiritual beliefs to help them overcome suicidal ideation
8. Agreeing: Essentially telling them that they should commit suicide.
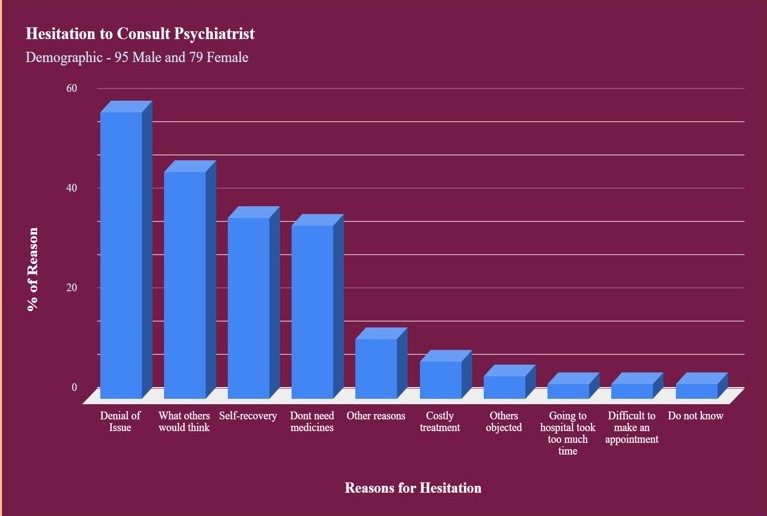
This graph shows the reasoning behind a possible hesitation to consult psychiatrists. The demographics are 95 Males and 79 Females. The most common reason is denial of issue, next to worries of perception of others.
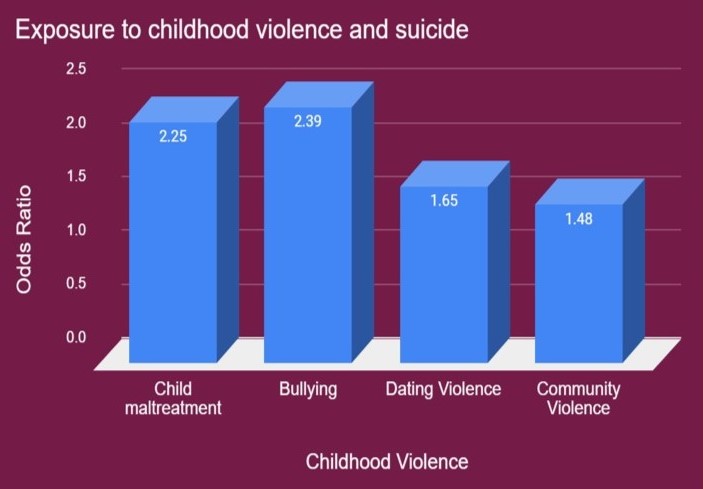
This graph shows the odds ratio of exposure to childhood violence and suicide. We can see that all of these have around two times
higher likelihood of having suicide attempts, than their counterparts who have not gone through these things.
Conclusion
The intricate and multifaceted nature of suicide demands a comprehensive approach that extends beyond relying solely on a single system for detection, identification, and prevention. The complexity of suicide, stemming from a myriad of interrelated factors including mental health conditions, social dynamics, economic stressors, and personal experiences, underscores the necessity of adopting holistic strategies within clinical settings to effectively combat this pressing issue.
A singular system, no matter how advanced, cannot adequately address the diverse array of risk factors and circumstances contributing to suicidal behavior. Instead, a holistic approach that integrates various disciplines, methodologies, and perspectives is essential. This approach should encompass not only clinical interventions but also community outreach, education, policy changes, and ongoing research efforts.
By embracing a holistic perspective, we recognize that suicide prevention is not a one-size-fits-all endeavor. It requires tailored interventions that acknowledge the unique needs and challenges faced by individuals at risk. Moreover, it emphasizes the importance of collaboration among mental health professionals, policymakers, educators, social workers, and other stakeholders to create a comprehensive network of support and resources.
Without a depth and variety of research into all aspects of suicide, our understanding remains incomplete, hindering our ability to develop effective prevention tactics. Every facet of this complex issue—from early warning signs and risk assessment to access to mental health services and societal stigma—must be thoroughly explored and addressed.
In conclusion, with dedicated research and analysis, my hope is that medical professionals, policymakers, and the youth of our generation will unite to find solutions for the pervasive issue of adolescent suicide. By comprehensively understanding the array of factors influencing mental health vulnerability and suicidal behavior, we can develop tailored interventions and support networks to protect the well-being of adolescents and cultivate a healthier future for all.
Citations
- https://pubmed.ncbi.nlm.nih.gov/27995627/
- https://www.sciencedirect.com/science/article/pii/S0005796719301056
- https://www.sciencedirect.com/science/article/abs/pii/S0165032711002412?via%3Dihub
- https://scholar.google.ca/scholar?q=psychological+factors+of+suicidal+ideation&hl=en&as_sdt=0&as_vis=1&oi=scholart
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7405877/
- https://www.ncbi.nlm.nih.gov/books/NBK220933/table/ttt00003/?report=objectonly
- https://www.ncbi.nlm.nih.gov/books/NBK220933/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3749837/
- https://pubmed.ncbi.nlm.nih.gov/35451317/#:~:text=Central%20to%20the%20psychoanalytic%20approach,self%2Dhate%2C%20and%20rage.
- https://journals.sagepub.com/doi/10.1177/00030651221086622?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
- https://link.springer.com/article/10.1007/s40473-019-00185-2
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6458543/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7405877/#bib88
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10046421/
- https://www.sciencedirect.com/science/article/pii/S0165032713005272
- https://www.nature.com/articles/s41380-021-01171-5
- https://nap.nationalacademies.org/read/10398/chapter/6#131
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6165520/
- https://www.ncbi.nlm.nih.gov/books/NBK220933/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7405877/
- https://www.sciencedirect.com/science/article/pii/S2352289523000541
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10046896/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533876/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8929755/
- https://uksobs.com/for-professionals/how-suicide-bereavement-is-different/?doing_wp_cron=1708994813.4212779998779296875000
- https://www.reddit.com/r/SuicideBereavement/
- https://www.sciencedirect.com/science/article/pii/S2666518221000371
- https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(14)70220-2/abstract#%20
- https://www.sciencedirect.com/science/article/abs/pii/S0306453016308435
- https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800342
Acknowledgement
Thank you to everyone who helped me throughout this project. Your work and contribution is greatly appreciated! I would like to mention by name:
- Dr. Meadow Schroeder, from the University of Calgary - Thank you for taking the time to help me brainstorm project ideas, help narrow down ideas, and help me connect the dots within my project.
- My Science Fair Coordinator, Ms. Deborah Rheinstein, Mr. Lahoda and other school teachers who have always supported, inspired and encouraged me
- My parents, for the never-ending support and helping me when I just needed to think my thoughts out loud, or when I needed help using technology!